 Case Report
Case Report
A Rare Case of HCV related Decompensated Cirrhosis complicated with Portopulmonary Hypertension
Richmond R Gomes1*, Nayeem Mehedi Aoyon2, Jannatul Moua Efa3, Rokeya Begum4 and Nafisa Rahman Bushra5
1Professor, Medicine, Ad-din Women’s Medical College Hospital
2,3Clinical Assistant, Medicine, Ad-din Women’s Medical College Hospital
4Medical Officer, Medicine, Ad-din Women’s Medical College Hospital
5Medical Officer, Medicine, Ad-din Women’s Medical College Hospital
Richmond Ronald Gomes, Professor, Medicine, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh
Received Date:April 15, 2025; Published Date:June 10, 2025
Abstract
Pulmonary arterial hypertension associated with portal hypertension, known as portopulmonary hypertension (PoPH) is one of the important and serious pulmonary complications in patients with portal hypertension. The prevalence of PoPH is about 0.25–4% among patients with cirrhosis. Although there are a large number of patients with portal hypertension due to mainly liver cirrhosis, the number of cases diagnosed with PoPH are far fewer because the causes of dyspnea in patients with cirrhosis are diverse and the disease entity of PoPH is poorly recognized by clinicians. Untreated PoPH can have a poor prognosis. We report here the case of 55 years old lady with hepatitis C (HCV) related decompensated cirrhosis complicated by PoPH.
Abbreviations: Portopulmonary hypertension; cirrhosis,; dyspnea; hepatitis C
Introduction
Pulmonary arterial hypertension associated with portal hypertension, known as portopulmonary hypertension (PoPH) is classified as a type of pulmonary artery hypertension (PAH) (subset of group 1 pulmonary hypertension [PH]). PoPH is one of the important and serious pulmonary vascular complication of cirrhotic and noncirrhotic portal hypertension and occurs in 2%-10% of these patients [1,2]. Although there are a large number of patients with portal hypertension due to mainly liver cirrhosis, the number of cases diagnosed with PoPH is far fewer because the causes of dys pnea in patients with cirrhosis are diverse and the disease entity of PoPH is poorly recognized by clinicians. Therefore, accurate assessment and suggestion of PoPH with noninvasive imaging are crucial. There is little evidence supporting the use of pulmonary arterial hypertension (PAH) therapies in patients with POPH because the overwhelming majority of clinical trials evaluating PAH‐specific therapies have excluded POPH patients3,4. We report here the case with PoPH suggested and assessed comprehensively by non-invasive transthoracic echocardiography. Unfortunately, the patient died during hospital course of treatment.
Case Report
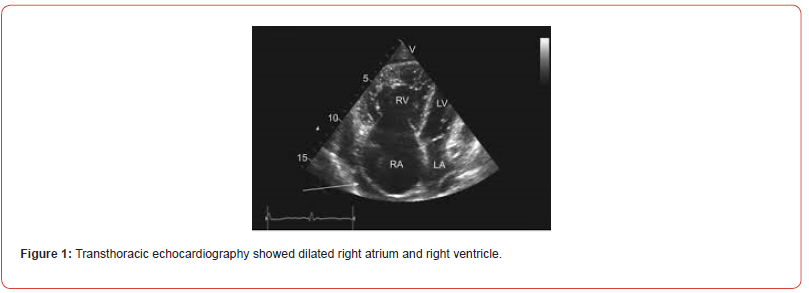
Mrs X, a 55 years old non diabetic, normotensive lady from Dhaka, Bangladesh is a known case of HCV related decompensated CLD (on velpatasvir and sofosbuvir combination) with portal hypertension (grade 2/3 esophageal varices with status post 2 session variceal band ligation) since 2020.This time she presented with graduation swelling of both leg and abdomen for 2 months and worsening shortness of breath and fatigue for 1 month. She denied any abdominal pain, chest pain, fever, altered sleep pattern, hematemesis, melana, orthopnea, weight loss, scanty micturition. On examination, she was conscious, oriented, dyspneic with respiratory rate 20 breaths /min, mildly anemic, mildly icteric. Jugular venous pressure was not raised. Bilateral pitting edema was present. Flapping tremor was absent. On abdominal examination, abdomen was hugely distended, non-tender. Ascites and splenomegaly were present. Cardiovascular system examination revealed evidence of pulmonary hypertension as evidenced by presence of palpable P2 and left parasternal lift. There was reduced air entry over both lung base. Sa02 was 91% in room air. Initial investigation revealed hemoglobin 8.2 gm/dl, MCV 102fl, white cell 3800/cmm, platelet count 84000/cmm. S. bilirubin 3.1 mg/dl, ALT 92 U/L, s. albumin 29.3 mg/dl, s. ammonia 12 micromol/L(normal below 30 micromol/L), prothrombin time patient 14 secs, control 12 secs, s. creatinine 0.83 mg/dl. Chest x ray showed bilateral mild pleural effusion with lung parenchymal lesion. USG of whole abdomen with doppler USG of portovenous system revealed moderate splenomegaly, huge ascites and dilated portal vein without evidence of any thrombus. Ascitic fluid study was noncontributory. Transthoracic echocardiography showed dilated right atrium (60 mm), dilated right ventricle (52 mm) and increased pulmonary arterial systolic pressure 65 mm of Hg at rest. There was no evidence of any valvular lesion (Figure 1). So, she was diagnosed as a case of portopulmonary hypertension and started treatment with tadalafil. Unfortunately, her condition deteriorated on tenth post admission day and she was shifted to intensive care unit. There she died on fourteenth post admission day.
Discussion
The diagnosis of PoPH requires demonstration of portal hypertension and precapillary PH with exclusion of other PH. POPH is defined as pulmonary hypertension that occurs as a consequence of portal hypertension with or without liver disease, and is a subset of group 1 pulmonary hypertension [3,4]. In the presence of documented portal hypertension, is defined according to the following hemodynamic data obtained during a RHC: (a) mean pulmonary artery pressure ≥20 mmHg; (b) PVR ≥2 Wood units; and (c) pulmonary artery wedge pressure ≤15 mmHg.3 In addition, the severity of POPH is defined based on the mPAP as follows: mild (20–34 mmHg), moderate (35–44 mmHg), and severe (≥45 mmHg). The vast majority of cases of POPH appear in patients with portal hypertension related to cirrhosis, but non‐cirrhotic causes of portal hypertension are also important contributors (portal vein thrombosis, granulomatous disease, auto‐immune disorders causing hepatitis, drug reactions, congenital abnormalities, and infections like chronic hepatosplenic shistosomiasis) [4]. Only 2%–6% of patients with portal hypertension also develop a pulmonary arterial hypertension [4]. In patients with POPH who had cirrhosis, pulmonary vascular bed is exposed to multiple circulating growth factors, neurohormone levels, and cytokine levels. Of particular importance are the increased levels of circulating endothelin‐1, a potent vasoconstrictor and facilitator of smooth muscle proliferation. On the other hand, pulmonary vascular bed may be deficient in local nitric oxide effect, a potent vasodilator [4].
High resolution pulmonary CT angiography, pulmonary perfusion imaging, myocardial LIE imaging, and ECV analysis, enables comprehensive evaluation of patients with PH [5]. This refined CT imaging protocol can be used in conjunction with standard chest evaluation and offers a practical and useful approach for the noninvasive “one-stop shop” evaluation of PH. Poor correlation exists between the severity of POPH and the degree of liver dysfunction and with hepatic venous pressure gradient [4]. Patients with POPH had poorer survival rates compared with patients with idiopathic or drug‐induced pulmonary hypertension (only 40% of patients after 5‐year time of diagnosis), and this could be because, in POPH, death can occur due to right failure or digestive complications (upper gastrointestinal bleeding, sepsis or hepatocellular carcinoma) [4]. The immediate goal in the treatment of POPH is to improve pulmonary hemodynamics by reducing the obstruction to pulmonary artery flow, improving and/or normalizing right ventricle (RV) function [3,4]. This can be accomplished by medications that result in vasodilatation and antiplatelet aggregation and have antiproliferative effects. There is little evidence supporting the use of pulmonary arterial hypertension therapies in patients with POPH, and it is known that in this type of pulmonary hypertension there is a delay in the initiation of treatment and more tendency to monotherapy [4]. In fact, the first randomized control trial in POPH (PORTICO), showed that macitentan gets a 35% reduction of PVR versus placebo and increases cardiac index, with no hepatic safety concerns [6]. Macitentan, a dual endothelin receptor antagonist, developed by modifying the structure of bosentan to increase efficacy and safety, demonstrated in the REPAIR study, by cardiac magnetic resonance imaging, an improvement in the structure and functionality of the RV, achieving an average increase in right ventricular stroke volume at week 26 with respect to the baseline value of 12 mL, a 10.6% increase in right ventricular ejection fraction, as well as a 38% decrease in PVR [7]. POPH is not an indication by itself for liver transplantation, being this procedure reserved for very selected cases.
Conclusion
Portopulmonary hypertension (PoPH) is one of the important and serious pulmonary complications in patients with portal hypertension. Untreated patients have serious consequences. Non-in invasive technique such as transthoracic echocardiography may serve as valuable screening tool in low resource settings. Multidisciplinary approach is needed to manage the cases.
Conflict of Interest
None declared.
References
- Chen HS, Xing SR, Xu WG, Yang F, Qi XL, et al. (2013) Portopulmonary hypertension in cirrhotic patients: prevalence, clinical features and risk factors. Exp Ther Med 5(3): 819-824.
- Hadengue A, Benhayoun MK, Lebrec D, Benhamou JP (1991) Pulmonary hypertension complicating portal hypertension: prevalence and relation to splanchnic hemodynamics. Gastroenterology 100(2): 520-528.
- Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, et al. (2022) ESC/ERS scientific document group. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 43: 3618-3731.
- Thomas C, Glinskii V, de Jesus PV, Sahay S (2020) Portopulmonary hypertension: from bench to bedside. Front Med (Lausanne) 7: 569413.
- Oda S, Kidoh M, Nagayama Y, Nakaura T, Hirakawa K, et al. (2021) Non-invasive imaging in pulmonary hypertension comprehensive assessment using dual-layer spectral computed tomography. Circ J 85(3): 316.
- Sitbon O, Bosch J, Cottreel E, Csonka D, de Groote P, et al. (2019) Macitentan for the treatment of portopulmonary hypertension (PORTICO): a multicentre, randomised, double‐blind, placebo‐controlled, phase 4 trial. Lancet Respir Med 7: 594-604.
- Noordegraaf AV, Channick R, Cottreel E, Kiely DG, Marcus JT, et al. (2022) The REPAIR study: effects of macitentan on RV structure and function in pulmonary arterial hypertension. JACC Cardiovasc Imaging 15(2): 240-253.
-
Richmond R Gomes*, Nayeem Mehedi Aoyon, Jannatul Moua Efa, Rokeya Begum and Nafisa Rahman Bushra.A Rare Case of HCV related Decompensated Cirrhosis complicated with Portopulmonary Hypertension. Acad J Gastroenterol & Hepatol. 4(2): 2025. AJGH.MS.ID.000585.
-
Portopulmonary hypertension; cirrhosis,; dyspnea; hepatitis C
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






