 Review Article
Review Article
Non-Patentable Chemicals for Cancer Therapy
Dmitriy Ovcharenko*, Dmitry Mukhin, and Galina Ovcharenko
Altogen Labs, Austin, Texas, USA
Dmitriy Ovcharenko, Altogen Labs, 11200 Menchaca Rd, Austin, TX 78748, USA
Received Date:March 14, 2024; Published Date:March 26, 2024
Abstract
A large number of chemicals are unpatentable within the current patent framework and the existing structure for protecting intellectual property in drug development. Anticancer compounds may be unpatentable because they are naturally occurring, lack novelty, or lack an inventive step, have insufficient evidence of efficacy, or fall under regulatory policies that prohibit patenting certain types of substances. Cancer researchers often discover new properties in existing compounds, but funding for basic research to determine their safety and efficacy is frequently unavailable because these compounds are unpatentable. Scientists commonly make modifications to the structure of unpatentable molecules in an attempt to make derivatives that can be patented instead of testing for effective and safe molecules that are not patentable. This article discusses the potential of non-patentable chemicals and the impact of relevant policies. A case study of dichloroacetate (DCA) role in cancer treatment demonstrates existing potential for developing novel anti-cancer compounds, despite the current structure of the patenting system that creates financial unviability of pursuing the research of non-patentable molecules. Testing efficacy and safety of unpatentable chemicals and their derivatives would expand access to more cancer therapeutic molecules and advance oncological research.
Keywords: Non-Patentable Chemicals; Cancer Therapy; Drug Development, DCA, DCAH, DCMAH
Introduction
Cancer is a leading global cause of death, but advances in technology and understanding of the disease are opening up opportunities for new drug discoveries. However, incorporating these new treatments into clinical practice is a lengthy process. It begins with the discovery of potential anticancer therapies and moves on to the assessment of their effectiveness and safety in a preclinical environment, aiming for regulatory approval to start clinical trials. In the USA, approval is granted by the United States Food and Drug Administration (US FDA). Subsequently, the drug development process includes three primary phases of clinical trials followed by a final compliance review. Altogether, the development of novel cancer drugs takes over decade and requires rigorous testing to determine their efficacy, toxicity, and pharmacological properties through laboratory and clinical studies. The estimated cost to develop and bring a new cancer drug to market exceeds a billion USD [1].
Patent protection is a key element in securing the costs of cancer drug development process, sponsors that typically range from large pharmaceutical companies to smaller biotech startups and even some academic ventures, choose not to pursue the development of a promising compound if it cannot be patented, as the absence of patent protection diminishes the financial incentive to invest in costly research and clinical trials, regardless of the compound’s therapeutic benefits. Also, not all patents are equally strong and frequent failure to follow subtle rules can significantly impact a patent’s value. Moreover, a large number of chemicals are part of the public domain and are non-patentable. The existing system of intellectual property protection implies that, without patents, patients will not be able to benefit from life sciences and medical research results because they are publicly available [2]. Manufacturers of non-patentable chemicals do not need to demonstrate safety or efficacy, and manufacturers cannot claim their products improve health or treat illnesses. Unfortunately, violations of this policy are not uncommon [3]. This creates a situation where there is no economic incentive for testing safety and efficacy, even in a preclinical setting.
The existing patenting system relies on the economic incentive for pharmaceutical and medical device companies that would lead to further investment into research and development, as well as innovative products to enhance healthcare. This perspective has been increasingly criticized within the last few decades [4]. Patents are criticized for obstructing healthcare by elevating the cost of vital medications, and hindering biomedical research by restricting access to essential patented materials. Public discussion and active participation of regulatory institutions led to new programs for expedited drug development [5], including the U.S. Orphan Drug Act that successfully delivered a number of novel treatments for rare cancers, of which some were subsequently used in other, nonorphan indications. Oncological drug development proves to be a major player in overall orphan drug research, displayed by more than one-third of all US FDA-approved orphan drugs with oncological indications [5,6].
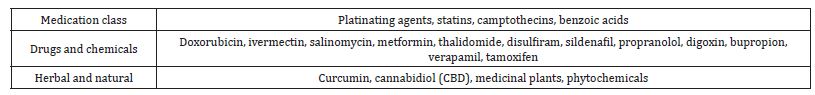
Unpatentable Compounds with Anti-Cancer Properties
Cancer therapy encompasses a diverse array of treatments aimed at combating malignant cell growth. Traditional modalities such as chemotherapy, radiation therapy, and surgery have long been cornerstones in cancer management. However, recent decades have witnessed a burgeoning interest in novel therapeutic approaches that target specific molecular pathways driving tumorigenesis. Non-patentable chemicals and off-patent drugs represent an important avenue in cancer therapy research and development. These compounds, which are not protected by patents and are often available as lower-cost alternatives to branded medications, have garnered significant interest for their potential in cancer treatment.
Many small molecules, metals and minerals have been used for centuries in cancer treatment, often in combination with other agents. Research studies demonstrated anti-cancer effects of arsenic that is associated with the cancer cell cycle arrest controlled by cyclins and cyclin-dependent kinases, followed by inducing apoptosis. Gold compounds can inhibit crucial enzymes like thioredoxin reductase, essential for cancer cell survival, leading to increased reactive oxygen species (ROS), causing oxidative stress and damaging cellular components, resulting in apoptosis. Gold compounds can disrupt key cellular signaling pathways and interact with DNA and RNA, impeding cancer cell replication. Additionally, studies demonstrated that gold may inhibit the formation of new blood vessels necessary for tumor growth and metastasis [7]. Selenium compounds exhibit anticancer effects by inducing oxidative stress in cancer cells, leading to DNA and cellular damage that promotes apoptosis. Conversely, at lower concentrations, selenium compounds demonstrate anti-inflammatory properties and enhances the body’s antioxidant defenses, helping to prevent DNA damage linked to cancer. It also modulates cell signaling pathways to promote cell death and inhibit cancer cell growth, migration, and invasion [8].
Since Rosenberg et al.’s discovery of the antitumor effects of cisplatin in 1969 [9], platinum-based complexes have remained a fundamental component of cancer chemotherapy. For over four decades, these agents, including cisplatin, carboplatin, and oxaliplatin, have been integral in the management of various cancer types, being mostly effective in ovarian, testicular, and head and neck cancers. Despite their proven efficacy, the clinical application of platinum-based drugs results in severe side effects such as gastrointestinal and nervous system toxicity, bone marrow suppression, and dose-limiting toxicities. Additionally, challenges such as partial tumor responses, drug resistance, and tumor relapse are prevalent, compromising long-term outcomes. These drawbacks have catalyzed ongoing research aimed at enhancing the therapeutic profiles of platinum therapies. A particularly promising direction in this endeavor is the development of nanocarrier-based delivery systems for platinum compounds. Platinates exert their mechanism of action primarily through the induction of platinum- DNA crosslinks, which disrupt the cancer cell’s DNA and trigger signal transduction pathways leading to cell death. Unfortunately, the clinical efficacy of platinum compounds is often undermined by resistance mechanisms, including reduced drug uptake, neutralization by cellular antioxidants, and enhanced capacities for DNA repair. Many research studies focused on elucidating these resistance pathways, identifying critical genes involved in resistance, and investigating the clinical side effects of platinumbased therapies. The advent of targeted cancer treatments has frequently incorporated platinates as cargo molecules in sophisticated delivery systems. Recent advances in nanotechnology have facilitated the development of Pt-based nanodrugs, which offer more targeted therapy options [10].
Salicylic acid and acetylsalicylic acid have well-known applications in medicine with demonstrated anticancer activity against melanoma via Akt/mTOR/AMPK-dependent activation of nitric oxide synthase 3 (eNOS). In both in vitro and in vivo models, salicylic acid triggered endoplasmic reticulum (ER) stress, which culminates with the upregulation of the pro-apoptotic transcription factor C/EBP homologous protein [11]. Salicylic acid has demonstrated anticancer potential by promoting apoptosis, inhibiting cell proliferation, modifying key enzymatic activities, disrupting cellular bioenergetics, and affecting inflammatory pathways. These combined effects suggest its utility in targeting various aspects of cancer progression.
Classic examples of non-patentable chemicals with antineoplastic properties are dimethyl sulfoxide (DMSO) and DCA. DMSO is a well-documented pharmaceutical solvent, utilized in various cancer therapy strategies, including Car-T cell therapy and Mekinist (trametinib DMSO), an US FDA approved treatment for melanoma. DMSO’s mechanism of action includes its ability to penetrate biological membranes, which enhances the absorption of other drugs, potentially increasing their efficacy. It also exhibits anti-inflammatory and analgesic properties, and can induce differentiation in certain cell lines, promoting more mature forms that are less aggressive and easier to target with therapy [12]. Despite its widespread use, current research has not fully explored DMSO’s potential to enhance the therapeutic effects of cancer treatments. While these small molecules themselves are not patentable, their analogs, specific formulations, or delivery methods might be (see Dichloroacetate case study section below).
Natural products have historically served as a vital source of bioactive compounds, significantly contributing to the discovery and development of pharmaceutical agents. Predominantly derived from terrestrial microbes, fungi, and plants, these natural products have been identified to contain numerous pharmacologically active agents. Several of these substances demonstrated anticancer properties. Natural products can be crucial contributors in oncological treatment strategies by exhibiting synergistic effects that enhance cancer therapy. Natural products represent a significant group of compounds that are typically excluded from patent eligibility within the current legal framework, primarily due to their natural origin [13]. These compounds frequently demonstrate variability in both production and composition, inherent to their natural derivation. Despite this variability, the anticancer efficacy of numerous natural products has been extensively documented in a variety of scientific studies. Furthermore, some literature reports suggests that the safety profiles of these natural compounds might be superior to those of their synthetic counterparts.
Camptothecin was first identified in the mid-60s by Wall and Wani. It showed promising anticancer effects, but the poor solubility and unpredictable side effects prevented the drug from being approved. Camptothecin is a naturally occurring, pentacyclic quinoline alkaloid that possesses high cytotoxic activity in a variety of cell lines. Camptothecin remains at equilibrium in an active lactone form and inactive hydrolyzed carboxylate form. The active lactone binds to DNA topoisomerase I cleavage complex, believed to be the single site of activity. Binding inhibits DNA religation, resulting in apoptosis. A series of small molecule camptothecin derivatives have been developed that increase solubility, lactone stability, and bioavailability to varying levels of success. A number of macromolecular agents have also been described wherein camptothecins are covalently appended or noncovalently associated with the goal of improving solubility and lactone stability, while taking advantage of the tumor physiology to deliver larger doses of drug to the tumor with lower systemic toxicity [14].
Adriamycin (ADM) has been effective against many types of solid tumors in clinical applications. However, its use is limited because of systemic toxicities, primarily cardiotoxicity, and multidrug resistance. A new active receptor-mediated complex, ADM conjugated with 2-amino-2-deoxy-d-glucose and succinic acid (2DG–SUC–ADM), was designed to target tumor cells through glucose transporter 1 (GLUT1). Researchers demonstrated that the complex had better inhibition rate to tumor cells and that ADM complex is capable to overcome multidrug resistance in cancer cells, indicating a promising drug for targeted cancer therapy [15].
Curcumin’s therapeutic potential in cancer treatment has been explored through numerous studies, which have emphasized its efficacy and potential mechanisms of action, despite the challenges posed by its low natural bioavailability and the development of resistance in cancer cells. Curcumin has been shown to suppress the expression of cyclin D1 in many types of cancer including colon, breast, bladder, head and neck, cervical, and pancreatic carcinomas. Anti-angiogenic properties and the role of curcumin in inducing apoptosis in cancer cells has also been extensively investigated. The anticancer effect is attributed to curcumin’s inhibition of NF-κB activation and subsequent suppression of downstream gene products [16]. Research efforts include the development of nanoparticles, lipid nanoemulsions, polymeric micelles, polymeric nanoparticles, solid-lipid nanoparticles, and other nanostructured lipid carriers designed to enhance curcumin’s bioavailability for chemotherapy applications. These advanced formulations have demonstrated promising results in optimizing particle size to ensure better absorption, stability, targeted delivery, biodistribution, and high drug loading capacities, providing efficient delivery of curcumin to target cancer cells. [17,18]. Moreover, curcumin was shown to influence the microRNA expression levels potentially providing novel therapeutic pathway in cancer treatment [19,20].
Over the past century, significant advancements in medicinal plant biotechnology and microbiology have led to the development of several anticancer phytomedicines. Modern pharmacopeia now comprises at least 25% of remedies based on herbal formulations, including clinically utilized anticancer drugs. Notable among these are drugs derived from podophyllotoxin, vinca alkaloids, curcumin, mistletoe plant extracts, taxanes, camptothecin, combretastatin, colchicine artesunate, homoharringtonine, ellipticine, roscovitine, maytansine, tapsigargin, and bruceantin. Additionally, a range of compounds such as psammaplin, didemnin, dolastin, ecteinascidin, and halichondrin have been isolated from marine organisms including microalgae, cyanobacteria, heterotrophic bacteria, and various invertebrates [21]. These compounds have undergone evaluations for their anticancer activities in cellular and experimental animal models and in few cases have been successfully incorporated into chemotherapy regimens.
Despite the variety of mechanisms of action exhibited by unconventional compounds, the prevailing patent system significantly limits their potential to be developed as cancer therapeutics. However, an established exception exists in the form of drug repurposing, which allows for the application of existing drugs to new therapeutic uses. Drug repurposing, also known as drug repositioning, is the process of identifying new therapeutic uses for existing drugs - those that are already approved for other health conditions. This approach can significantly reduce the time and cost associated with drug development because it leverages existing data on the drug’s safety, pharmacokinetics, and potential side effects. Drug repurposing is appealing because it can bring treatments to market faster, providing new effective therapy options. This method is especially valuable in oncology, offering a quicker, cost-effective development process by utilizing existing data on drug safety, dosage, and toxicity [22].
Dichloroacetate Case Study
DCA is an example of a non-patentable chemical that was studied by Otto Warburg back in the 1920s relating to cancer physiology (in particular the associated buildup of lactate). The chemical compound has a relatively complicated function in living cells. One of its first early uses several decades ago was to treat the buildup of lactate in human tissues [23]. In recent years, DCA has been studied in connection to cancer research and a number of reports demonstrated promising anti-cancer activity, suggesting its use in clinical trials as an anti-cancer treatment [24,25]. DCA, identified as a pyruvate dehydrogenase kinase (PDK) inhibitor, instigates a metabolic transition in cancer cells from glycolysis to oxidative phosphorylation, counteracting the Warburg effect that characterizes the altered metabolism of cancerous cells. This metabolic shift not only induces apoptosis in cancer cells but also enhances their susceptibility to conventional treatments, offering a novel approach to cancer therapy. A number of in vitro studies linked the compound to the inhibition of breast cancer [26], colon cancer [27], prostate cancer [28], glioblastoma [29], lung cancer [30], leukemia [31], and other types of cancer (Table 1).
Table 1: Selected Reports of DCA Anticancer Effects Against Different Types of Cancer.
Studying DCA’s mechanism of action revealed it functions as an inhibitor of PDK, effectively reversing the Warburg effect and inducing tumor cell death. Despite its potential, studies on DCA’s anti- cancer properties have highlighted the necessity for high dosages and documented instances of toxicity [32]. Showing promise, DCA was tested in an initial clinical trial, but the compound’s toxic effects prevented it from becoming a common and affordable cancer therapeutic [33]. Despite DCA’s promising preclinical anticancer efficacy, its transition to clinical application has been restrained by concerns over its neurotoxicity, however there is a clinical potential for DCA analogs or when used in synergy with chemotherapy, radiotherapy, and other anticancer agents, to amplify therapeutic efficacy while mitigating toxicity. Synergistic effects observed when DCA is combined with various chemotherapeutic agents across different cancer models were demonstrated with improved treatment outcomes and the ability to circumvent chemoresistance [33]. It elaborates on the integration of DCA with other potential anticancer drugs and natural compounds, highlighting instances of enhanced anticancer activity and reduced adverse effects, thereby presenting a compelling case for the combinatory use of DCA in oncology.
The effect of DCA on cancer stem cells (CSCs) demonstrated potential to target this notoriously resilient cancer cell population. By modulating the metabolic profile of CSCs, DCA presents a promising strategy to prevent tumor relapse, addressing one of the paramount challenges in cancer treatment [33]. Further development suggested DCA combinatorial use with traditional cancer treatments, testing new delivery methods for DCA therapy, and subsequent testing of DCA analog compounds [34].
The study of DCA alternatives evaluated eight small compounds with a conserved dichloric terminal for their in vitro and in vivo potential for anticancer activity [34]. Two compounds out of the initial eight ended up substantially reducing tumor growth. Data demonstrated that cationic dichloric compounds 2,2-dichloroethan- 1-amine hydrochloride (DCAH) and (2,2-dichloroethyl)(methyl) amine hydrochloride (DCMAH) inhibit tumor growth in the U87 xenograft model of glioblastoma, suggesting their clinical potential as accessible anti-cancer drugs. Studies of cationic DCAH and DCMAH molecular mechanism of action demonstrated that analog compounds are likely to be different from that of the terminally carboxylic DCA, highlighting the need for further investigation to fully understand their therapeutic potential.
DCA and its analogs sparked an interest and received certain attention from the scientific community. However, most other classes of non-patentable chemical molecules are unlikely to be developed or even tested as potential cancer drugs due to the existing patenting structure and associated lack of funding. Under the existing structure for protection of intellectual property in drug development, the financially justified research choice is limited to modification of the structure of non-patentable molecules in an attempt to make derivatives that can be patented, instead of testing for effective and safe molecules that are not patentable. This structure limits the expansion of safe chemical molecules available to advance scientific research, as it is financially nonviable to pursue. If adequate grant funding was made available, it would create an opportunity to investigate the potential of molecules such as DCA and DCA analogs within the structure of the current patenting system. Consequently, this would expand understanding of safety and anticancer efficacy of many non-patentable compounds, providing more therapeutic options to advance oncological research and cancer treatment.
Acknowledgement
None.
Conflict of Interest
No Conflict of Interest.
References
- Nosengo N (2016) Can you teach old drugs new tricks? Nature. 534(7607): 314-316.
- Root-Bernstein RS (1995) The development and dissemination of non-patentable therapies (NPTs). Perspect Biol Med. 39(1): 110-7.
- Brown AC (2017) An overview of herb and dietary supplement efficacy, safety and government regulations in the United States with suggested improvements. Part 1 of 5 series. Food Chem Toxicol 107(Pt A):449-471.
- Gold ER, Kaplan W, Orbinski J, Harland-Logan S, N-Marandi S (2010) Are patents impeding medical care and innovation? PLoS Med 7(1): e1000208.
- Brown DG (2024) A Drug Discovery Perspective on FDA Expedited Development and Incentive Programs. J Med Chem 67(3): 1690-1700.
- Stockklausner C, Lampert A, Hoffmann GF, Ries M (2016) Novel Treatments for Rare Cancers: The U.S. Orphan Drug Act Is Delivering-A Cross-Sectional Analysis. Oncologist 21(4): 487-93.
- Yue S, Luo M, Liu H, Wei S (2020) Recent Advances of Gold Compounds in Anticancer Immunity. Front Chem 8: 543.
- Radomska D, Czarnomysy R, Radomski D, Bielawski K (2021) Selenium Compounds as Novel Potential Anticancer Agents. Int J Mol Sci 22(3): 1009.
- Rosenberg B, VanCamp L, Trosko J E, Mansour V H (1969) Platinum compounds: a new class of potent antitumour agents. Nature 222: 385-386.
- Zhang C, Xu C, Gao X, Yao Q (2022) Platinum-based drugs for cancer therapy and anti-tumor strategies. Theranostics 12(5): 2115-2132.
- Ausina P, Branco JR, Demaria TM, et al. (2020) Acetylsalicylic acid and salicylic acid present anticancer properties against melanoma by promoting nitric oxide-dependent endoplasmic reticulum stress and apoptosis. Sci Rep 10(1): 19617.
- Hoang BX, Han BO, Fang WH, Tran HD, Hoang C, et al. (2023) The Rationality of Implementation of Dimethyl Sulfoxide as Differentiation-inducing Agent in Cancer Therapy. Cancer Diagn Progn. 2023 Jan 3;3(1): 1-8.
- Sahoo A, Mandal AK, Kumar M, Dwivedi K, Singh D (2023) Prospective Challenges for Patenting and Clinical Trials of Anticancer Compounds from Natural Products: Coherent Review. Recent Pat Anticancer Drug Discov 18(4): 470-494.
- Venditto VJ, Simanek EE (2010) Cancer Therapies Utilizing the Camptothecins: A Review of the in Vivo Literature. Mol Pharmaceutics 7(2): 307-349.
- Cao J, Cui S, Li S, et al. (2013) Targeted Cancer Therapy with a 2-Deoxyglucose–Based Adriamycin Complex. Cancer Research 73(4): 1362-1373.
- Wilken R, Veena MS, Wang MB, Srivatsan ES (2011) Curcumin: A review of anti-cancer properties and therapeutic activity in head and neck squamous cell carcinoma. Mol Cancer 10:12.
- Jacob S, Kather FS, Morsy MA, Boddu SHS, Attimarad M, et al. (2024) Advances in Nanocarrier Systems for Overcoming Formulation Challenges of Curcumin: Current Insights. Nanomaterials (Basel) 14(8): 672.
- Baoum A, Ovcharenko D, Berkland C (2012) Calcium condensed cell penetrating peptide complexes offer highly efficient, low toxicity gene silencing. Int J Pharm 427(1): 134-42.
- Cao M, Duan Z, Wang X, Gong P, Zhang L, (2024) Curcumin Promotes Diabetic Foot Ulcer Wound Healing by Inhibiting miR-152-3p and Activating the FBN1/TGF-β Pathway. Mol Biotechnol 66(5): 1266-1278.
- Sachse C, Krausz E, Krönke A, Hannus M, Walsh A, (2005) High-throughput RNA interference strategies for target discovery and validation by using synthetic short interfering RNAs: functional genomics investigations of biological pathways. Methods Enzymol 392: 242-77.
- Pathak K, Pathak MP, Saikia R, Gogoi U, Sahariah JJ, et al. (2022) Cancer Chemotherapy via Natural Bioactive Compounds. Curr Drug Discov Technol 19(4): e310322202888.
- Zhang Z, Zhou L, Xie N. et al. (2020) Overcoming cancer therapeutic bottleneck by drug repurposing. Sig Transduct Target Ther 5(1): 113.
- Kreisberg RA (1980) Lactate homeostasis and lactic acidosis. Ann Intern Med 92(2 Pt 1): 227-37.
- Michelakis ED, Webster L, Mackey JR (2008) Dichloroacetate (DCA) as a potential metabolic-targeting therapy for cancer. Br J Cancer 99: 989-994.
- Bonnet S, Archer SL, Allalunis-Turner J, Haromy A, Beaulieu C, et al. (2007) A mitochondria-K+ channel axis is suppressed in cancer and its normalization promotes apoptosis and inhibits cancer growth. Cancer Cell. 11:37-51.
- Wang M, Liao C, Hu Y, Qinwen P, Jiang J (2017) Sensitization of breast cancer cells to paclitaxel by dichloroacetate through inhibiting autophagy. Biochem Biophys Res Commun. 489: 103-108.
- Khan A, Andrews D, Blackburn AC (2016) Long-term stabilization of stage 4 colon cancer using sodium dichloroacetate therapy. World J Clin Cases 4: 336-343.
- Cao W, Yacoub S, Shiverick KT, Namiki K, Sakai Y, et al. (2008) Dichloroacetate (DCA) sensitizes both wild-type and over expressing Bcl-2 prostate cancer cells in vitro to radiation. Prostate. 68: 122-1231.
- Shen H, Decollogne S, Dilda PJ, Hau E, Chung SA, (2015) Dual-targeting of aberrant glucose metabolism in glioblastoma. J Exp Clin Cancer Res 34: 14.
- Fiebiger W, Olszewski U, Ulsperger E, Geissler K, Hamilton G (2011) In vitro cytotoxicity of novel platinum-based drugs and dichloroacetate against lung carcinoid cell lines. Clin Transl Oncol 13: 43-49.
- Qin L, Tian Y, Yu Z, Shi D, Wang J, et al. (2016) Targeting PDK1 with dichloroacetophenone to inhibit acute myeloid leukemia (AML) cell growth. Oncotarget 7:1395-1407.
- Stacpoole PW, Martyniuk CJ, James MO, Calcutt NA (2019) Dichloroacetate-induced peripheral neuropathy. Int Rev Neurobiol 145:211-238.
- Tataranni T, Piccoli C (2019) Dichloroacetate (DCA) and Cancer: An Overview towards Clinical Applications. Oxid Med Cell Longev. 8201079.
- Ovcharenko D, Chitjian C, Kashkin A, Fanelli A, Ovcharenko V (2019) Two dichloric compounds inhibit in vivo U87 xenograft tumor growth. Cancer Biol Ther 20(9): 1281-1289.
- Harting T, Stubbendorff M, Willenbrock S, Wagner S, Schadzek P, et al. (2016) The effect of dichloroacetate in canine prostate adenocarcinomas and transitional cell carcinomas in vitro. International Journal of Oncology 49: 2341-2350.
- Michelakis ED, Sutendra G, Dromparis P, Webster L, Haromy A, et al. (2010) Metabolic modulation of glioblastoma with dichloroacetate. Sci Transl Med 2(31): 31ra34.
- Al-Azawi A, Sulaiman S, Arafat K, Yasin J, Nemmar A, et al. (2021) Impact of Sodium Dichloroacetate Alone and in Combination Therapies on Lung Tumor Growth and Metastasis. Int J Mol Sci 22(22):12553.
- Agnoletto C, Melloni E, Casciano F, Rigolin GM, Rimondi, et al. (2014) Sodium dichloroacetate exhibits anti-leukemic activity in B-chronic lymphocytic leukemia (B-CLL) and synergizes with the p53 activator Nutlin-3. Oncotarget 5(12): 4347-60.
- Sorokina LV, Pyatchanina TV, Didenko GV, Kaplia AA, Khyzhnyak SV (2011) The influence of sodium dichloroacetate on the oxidative processes in sarcoma 37. Exp Oncol 33(4): 216-21.
- Klose K, Packeiser EM, Müller P, Granados-Soler JL, Schille JT, et al. (2021) Metformin and sodium dichloroacetate effects on proliferation, apoptosis, and metabolic activity tested alone and in combination in a canine prostate and a bladder cancer cell line. PLoS One 16(9): e0257403.
- Sun J, Cheng X, Pan S, Wang L, Dou W, et al. (2021) Dichloroacetate attenuates the stemness of colorectal cancer cells via trigerring ferroptosis through sequestering iron in lysosomes. Environ Toxicol 36(4): 520-529.
- Flavin DF (2010) Non-Hodgkin's Lymphoma Reversal with Dichloroacetate. J Oncol 414726.
- Tataranni T, Agriesti F, Pacelli C, Ruggieri V, Laurenzana I, et al. (2019) Dichloroacetate Affects Mitochondrial Function and Stemness-Associated Properties in Pancreatic Cancer Cell Lines. Cells 8(5): 478.
- Sun L, Jiang Y, Yan X, Dai X, Huang C, et al. (2021) Dichloroacetate enhances the anti-tumor effect of sorafenib via modulating the ROS-JNK-Mcl-1 pathway in liver cancer cells. Exp Cell Res 406(1): 112755.
- Zhang X, Lee WD, Leitner BP, Zhu W, Fosam A, et al. (2023) Dichloroacetate as a novel pharmaceutical treatment for cancer-related fatigue in melanoma. Am J Physiol Endocrinol Metab 325(4): E363-E375.
- Tian DD, Bennett SK, Coupland LA, Forwood K, Lwin Y, et al. (2019) GSTZ1 genotypes correlate with dichloroacetate pharmacokinetics and chronic side effects in multiple myeloma patients in a pilot phase 2 clinical trial. Pharmacol Res Perspect 7(6): e00526.
-
Dmitriy Ovcharenko*, Dmitry Mukhin, and Galina Ovcharenko. Non-Patentable Chemicals for Cancer Therapy. Adv Can Res & Clinical Imag. 4(2): 2024. ACRCI.MS.ID.000584.
-
Non-Patentable Chemicals; Cancer Therapy; Orphan Drugs; DCA; DCMAH
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






