 Opinion
Opinion
Consumer Health Informatics for Cancer Treatment Engagement
Margaret Czart1* and Dick Lui2
1DrPH, Biomedical and Health Information Sciences, University of Illinois Chicago, USA
2MPH, Biomedical and Health Information Sciences, University of Illinois Chicago, USA
Margaret Czart, DrPH, University of Illinois Chicago, 1919 Taylor Street, 263ASHB, MC 530, Chicago, Il, 60612, USA.
Received Date: March 24, 2023; Published Date: April 03, 2023
Abstract
Cancer is defined by the National Cancer Institute as a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body. Often cancers may start in any part of the body and begin with small tumors [1]. Engagement of a patient with a cancer diagnosis is determined by an individual’s belief that they have a problem and what action they are willing to take. The field of Consumer Health Informatics (CHI) represents new possibilities for healthcare delivery as a framework for more personalized and holistic healthcare that fosters active selfmanagement of one’s state of health in terms of both remediating health dysfunction and promoting wellness. Every patient goes through the initial issues of health belief and transtheoretical stages of changes in life. Engagement of a patient with a cancer diagnosis is determined by an individual’s belief that they have a problem. Current work in these topics independently shows that cancer consumers/patients are open to technology for many aspects of everyday life. However, the challenges occur when addressing various types of cancers due to each situation being different. The needs for health information and the type of health information are different. Innovative technologies such as Augmented Reality (AR) which uses both mobile applications and paper target images. Cancer patients and caregivers may be willing to test innovative AR technology by downloading a mobile application and be provided with target images that may be printed out and view the material for educational purposes. Educational programs can be developed to continue the engagement started by the physician. By using AR and VR tools, engagement can extend beyond the exam room and into the world.
Keywords: Consumer health informatics; Patient engagement; Health literacy; Digital literacy
Introduction
Cancer is defined by the National Cancer Institute as a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body. Often the cancers may start in any part of the body and begin as small tumors [1]. For patients (disease management) and caregivers the diagnosis of disease through various medical examinations and tests is considered a devastating diagnosis. Every patient goes through the initial issues of health belief and transtheoretical stages of changes in life. Diagnosis of a patient with a cancer diagnosis is determined by an individual’s belief that they have a problem and what action they are willing to take. In today’s digital society the need to understand all types of cancers as a disease and the treatment options (traditional and innovative) are growing as patients and their caregivers become increasingly involved in decision-making in an interprofessional value-based care system. However, there is a need for educational material which is accessible, understandable, and engaging in a digital society by all cancer patients. However, many patients still encounter challenges in health literacy and digital literacy for accessing, retrieving, and engaging with what is known about various cancers. Therefore, cancer patients and caregivers need educational material, which is understandable, accessible, and engaging at the individual patient’s health and digital literacy skill levels. Therefore, the question remains on how Consumer Health Informatics Professionals may assist Oncologists, Radiologists, and other health professionals in assisting Cancer Patients in staying engaged in the treatment process using various technologies available to patients with the assistance of Consumer Health Informatics Professionals in today’s digital society.
Defining the Role of Consumer Health Informatics Professionals
The field of Consumer Health Informatics (CHI) represents new possibilities for healthcare delivery as a framework for more personalized and holistic healthcare that fosters active selfmanagement of one’s state of health in terms of both remediating health dysfunction and promoting wellness. Specifically, it is the area of health informatics which includes patient-focused informatics, health literacy and consumer education. The focus is on information structures and processes that empower consumers to manage their own health through health information literacy, consumer-friendly language, personal health records, and Internetbased strategies and resources. The term “Consumer” in Health informatics refers to patient, citizen, resident, advocate, community member, stakeholder, individual, person, human, caregiver, family member, and end user [2]. Traditionally, CHI professionals create health educational materials across various traditional 2D to innovative 3D technology platforms. The goals are to address health and digital literacy of patients and caregivers through health education and promotion while collaborating with professionals to address specific cancer patient needs. These include the evaluation and adoption of various technologies by patients and caregivers to validate the best practices of accessing and retrieving information without putting themselves at risk to health professional impersonators which patients often refer to as their “Health Guru” providing treatment options which are not necessarily in the best interest of the patient. Both patients and their families may not necessarily have the skills to differentiate valid health information from invalid information found using internet websites, mobile applications and social media platforms.
Consumer Health Engagement Frameworks Applied to Cancer
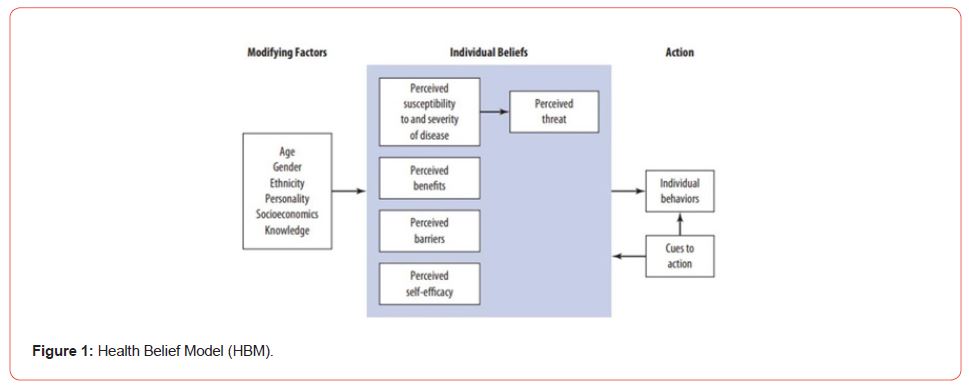
For consumers (disease-prevention) and patients (disease management) the diagnosis of cancer at any stage through various medical examinations and tests is considered a devastating diagnosis. Every patient goes through the initial issues of health belief and transtheoretical stages of changes in life. Engagement of a patient with a cancer diagnosis is determined by an individual’s belief that they have a problem. The Health Belief Model focuses on the perceived susceptibility, perceived severity, perceived benefits, and barriers to engaging in a behavior, cues to action, and self-efficacy. The cancer patient’s belief is based on 1) the personal susceptible to a condition (at risk for a disease), 2) how potentially serious consequences, 3) potential action (behavior) available to them could be of benefit in the situation getting worse, 4) understanding the benefits to acting, and 5) perspective on perceived barriers (or costs) are outweighed by the benefits [3]. For example, patients and their families are often aware of the potential benefits and side effects of traditional treatments of chemotherapy and radiation. However, the hesitation if the treatment will work and the potential consequences are of high importance. At the same time the option of new innovative treatments such as Radioembolization (Y90) for liver cancer brings hope as a minimal invasive treatment and hesitation if the benefits outweigh the risks. Some of the most common risks range from stomach ulcers to blood vessel damage, and infection [4]. The health belief model is often closely related to the Transtheoretical Model of Change, which is a process that unfolds over time, progressing through a series of stages going from Precontemplation (no action), Preparation for action, Action, and Maintenance (maintaining treatment/ action). Often patients may go through these stages several times throughout the treatment process [5]. For example, an individual may be at the preparation stage for a long period of time, that by the time they decide on treatment it may be too late and treatment options are limited (Figure 1).
Patient Engagement regarding technology use for health information/education will be determined based on technology acceptance of health behavior change which is known as the Technology Acceptance Model (TAM). The framework had been influential to determine factors affecting users’(patient’s) acceptance of a given technology based on perceived ease of use and usefulness in association between system characteristics (external variables) and technology usage for the purpose of their interest (Figure 2).
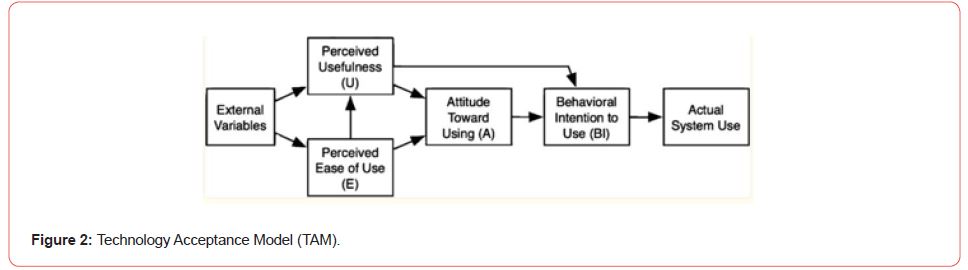
For cancer patients this may be to retrieve information about their specific types of cancer, learning about their treatment options, building community with other cancer patients, and learning about other cancer patient success stories. Based on the information and understandability of the information presented to a patient and their caregivers will determine the action they would potentially pursue as the best option. Often patients and their caregivers may not be quick on deciding on a specific action. Therefore, there is a need to explore the options of innovative technologies to assist in engaging patients early to increase the probability of early action rather than waiting. Technology offers written communication which may be more influential than any verbal communication by professionals based on the patient perceived fee for service health care mode (Figure 2).
The various frameworks all require patients to accept and believe that something is helpful and useful. The Health Belief and Transtheoretical Models focus on human belief and behavior change while the design of technology is influential to getting patients to accept technology to supplement health behavior change. All the frameworks address the belief to either the health issue or technology. In today’s digital society both together may improve outcomes and convince a cancer patient early enough to obtain treatment. However, at times the cancer patient alone will not consider cancer treatment beneficial. Other individuals such as family members who may also serve as caregivers may be the influential factor to address the issue early. Therefore, the knowledge and beliefs of caregivers for the most appropriate actions in the decision-making process for cancer treatment should not be underestimated. The health literacy level may be higher for caregivers to take the role of consumer health professionals to explain various benefits and options to the cancer patient. In turn, the cancer patient may be more likely to believe the caregiver/ family member as they trust the best interest of the patient to be considered.
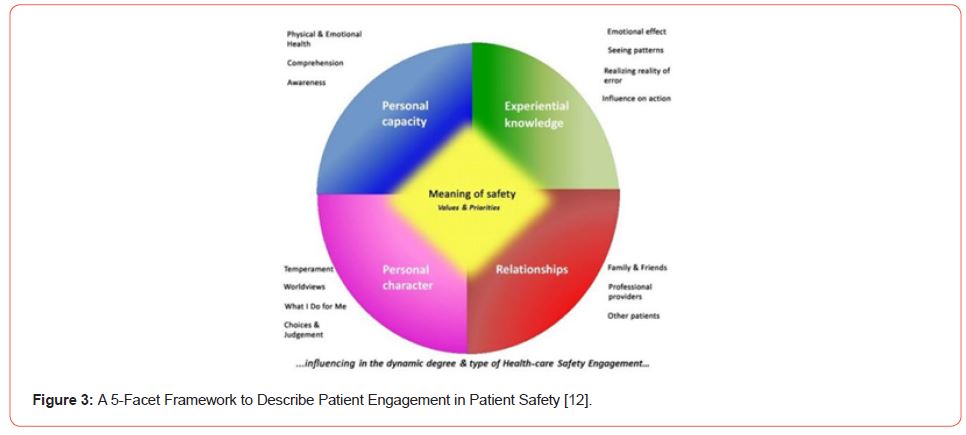
Caregivers play a key role and may assist with providing the proper support access and retrieve information based on their potentially higher digital literacy skills. According to Duhn and Medves there are five facets for patient safety and decision making on health care services based on five facets which contribute the meaning of patient safety from the patient perspective when considering engagement in addressing health issue (Figure 3) [12]. The facets are identified as Personal Capacity; Experiential Knowledge; Personal Character; Relationships; and Meaning of Safety. Cancer patients may often feel confused as it is critical to understand the various stages of cancer and what the options are for treatment. This is especially true for those who may have knowledge of a family history of cancer in the family. Typically, cancers such as breast, ovarian, uterine, or colorectal may be hereditary [6]. As one member obtains a diagnosis others may get tested as well. The knowledge of a family history may bring insight to how engaged someone is willing to fight the disease. However, in cases where there is no known history of cancer there will be a moment of denial, wanting a second opinion, looking for information to prove otherwise. Family members often do their best to provide support but are hesitant to provide a recommendation which may not work. Finally, there may be cases where the family does their best to convince a patient to agree to treatment which at times may allow a cancer to spread (Figure 3).
Challenges of Consumer Health Vocabulary and Technology Tools
Today, there are various traditional 2D technologies used for cancer health promotion and education for patients and caregivers. These include the traditional patient portals/personal health records, web browser/search engines, social media groups, and mobile applications. It is critical for health information.
consumers to develop the health information literacy skills to not only access or retrieve information, but to evaluate its credibility, as well as the credibility of information resources. In the same sense that that the Electronic Health Records is an enabling technology for Health Informatics, the concept of the personal health record is the keystone for integrating the consumer health information needs of stakeholders with health information technologies. However, the management of quantitative and qualitative data in pieces becomes a challenge. Patient Portals lack explanations of various terminologies. Therefore, the importance of medical terminology among professionals is vital to further improve health and data literacy among patients and consumers. Open notes have provided cancer patients with access to physician notes after a clinical visit. However, cancer patients search for additional health information to understand their own health status using various tools. The use of search engines such as Google, Yahoo and Bing are one of the first locations a patient may use to search for health information. Understanding the consumers health information seeking behavior is critical to addressing the issues of access to health information and the quality of the health information. Demonstrating the ability to identify valid from non-valid information is important for patient safety. Therefore, there is a need for further development of the consumer health vocabulary (CHV) which was first proposed in 2001 and expanded in 2007. Many cancer patients and others are dependent on consumer terms to be mapped to the UMLS medical terms. The expanded CHV will help cancer patients and caregivers expand their health literacy of medical terminology and potentially improve health outcomes through improved decisionmaking [7]. According to Morselize and colleagues the last CHV update included other additional health social behaviors such as vaping which is linked to lung cancer. Finally, the usability design is critical to an individual’s ability to use specific tools effectively. This is especially true if something looks different on a desktop vs. mobile device. However, there will always be a group of patients who are hesitant about technology in health care until they are convinced by personal experience and/or trust of someone they know. At the same time, there will be other patients who will be afraid of new technology until the step-by-step instructions are provided and they may try using it with someone’s assistance. The lack of Consumer Health Professionals in the field makes it difficult to assist patients in building digital literacy skills to build the appropriate technical skills to access and understand health information moving to the digital online environment. In addition, many patients will prefer to select only one preferred technology tool as their primary source of health information/education on cancer. The design of technology and how information is presented through the Technology Acceptance Model may influence a patient’s and caregivers’ decision on cancer treatment. Technology may build a trust factor which is not necessarily achievable in the physician-patient/caregiver relationship.
Effective Patient Engagement
Patients can experience a range of emotions while receiving care for cancer. After receiving a cancer diagnosis, it is common for patients report going into shock and experiencing a state of “numbness.” Physicians expect this reaction from patients and prepare for it by including a family member for social support when talking to a patient about a new diagnosis and prognosis. However, while shock is a common reaction for patients, not all patients experience shock. Some patients report having feeling of validation or relief upon receiving a cancer diagnosis [8]. Additionally, while it is a customary practice to have a close companion accompany the patient, one study found that while 50% of respondents preferred having a spouse with them when the diagnosis of cancer was communicated, 38% preferred to be alone [9]. So, patients have a wide variety of engagement preferences. Consumer health engagement frameworks can help physicians communicate more effectively with patients. Physicians use various techniques like medical interviewing and motivational interviewing and approaches like “ask-tell-ask” and “tell me more” to engage with patients [10]. While these techniques can be effective, consumer health engagement frameworks can be used to assess and stage the patient. For instance, if the physician needs to engage the patient to make an informed decision about treatment, the engagement will differ if the patients wanted more knowledge about the effectiveness of the treatment compared to having anxiety about the treatment’s side effects. These frameworks can help tailor the messages in these techniques to the patient’s educational needs and engagement preferences and deliver them to the physician through CPOE alerts. Tools like AR also be used for decision making. AR has already been used in retail to show how consumers might look like wearing clothes or eyeglasses. The same can be employed for breast cancer survivors considering reconstructive surgery.
Effective Consumer Engagement
Consumer engagement is focused on prevention. Prevention messages promote screening and preventative lifestyles. However, traditionally, prevention messages target populations. During an exam, primary care providers also use medical interviewing and motivational interviewing if patients are resistant to screening but including the use of consumer health engagement frameworks, CPOE can also offer guide the provider to understand why patients may be resistant. Do they have low susceptibility? Do they carry a belief that screening offers low benefits therefore is not worth the time? Targeting patients’ specific needs can make the best use of limited time during an exam. Given the limited time during an exam. Consumer health engagement tools like patient portals and personal health record systems and continue to educate consumers after the exam. Educational programs can be developed to continue the engagement started by the physician. By using AR and VR tools, engagement can extend beyond the exam room and into the world. Consumers can practice shopping in a virtual grocery store to practice healthy food selection and that experience can be extended by providing the consumer with video recipes.
Health Technology Limitations for the Cancer Consumer/Patient Model
The stakeholders referred to as “Consumers” are individuals such as patients, citizens, residents, advocates, community members, individuals, persons, humans, caregivers, family members, end users [2]. Current work in these topics independently shows that cancer consumers/patients are open to technology for many aspects of everyday life. However, the challenges occur when addressing various types of cancers due to each situation being different. The needs for health information and the type of health information are different. How easy it is to access health information is also an issue. This is mainly due to issues associated with technology design where the adoption and evaluation of a given tool alone is not enough. This is often referred to as technology design thinking which makes assumptions on user needs. Oncologists with the collaboration of Consumer Health Informatics professionals need to consider how a given technology is used by various types of cancer patients and for what purpose. For example, we need to consider not only is health information understandable and assessable on a given technology tool but also is the right technology tool used appropriately for the type of information that is presented. In considering the human-computer interaction with technology the assessment of usability needs to assess the information presented. For example, a website on various cancers may provide standard qualitative textual information describing the disease and quantitative statistics. Innovative technologies such as Augmented Reality (AR) which uses both mobile applications and paper target images. Cancer patients and caregivers may be willing to test innovative AR technology by downloading a mobile application and be provided with target images that may be printed out and view the material for educational purposes. In some AR applications such as OSF “About Me 3D” also provide a short story as part of the target image [11,12]. Animated stories using innovative technologies may assist as health education tools and what to expect during the cancer treatment process. Often patients won’t admit what they don’t understand.
Conclusion
From the work accomplished through this discussion has several key lessons which need to be addressed. The lessons learned include 1) Importance of various traditional frameworks influence a patient and caregivers’ approach to cancer treatment, 2) Importance of health literacy, data literacy and technology design for health information access and education, 3) Need for Consumer Health Informatics Professionals needed to focus on patient and caregiver needs to improve health outcomes during the treatment process.
Acknowledgement
None.
Conflict of Interest
No Conflict of Interest.
References
- National Cancer Institute (2023). What is Cancer?
- American Medical Informatics Association (2022) Consumer Health Informatics.
- Skinner S, Trio J, Champion V (2015) The Health Belief Model. In: Glanz K (Ed.) (5th edn.). Health Behavior: Theory, Research and Practice. San Francisco, CA, Jossey-Bass Publishing. pp.75-94.
- Radiology Info (2022). Radioembolization (Y90).
- Prochaska J, Redding C, Evers K (2015) The Transtheoretical Model and Stages of Change. In: Glanz K (Ed.) (5th edn.). Health Behavior: Theory, Research and Practice. San Francisco, CA, Jossey-Bass Publishing. pp.125-143.
- (2022) Centers for Disease Control and Prevention. Family Health History and Cancer.
- Monselise M, Greenberg, Ou Stella Liang, Sonia Pascua, Heejun Kim, et al. (2021) An Automatic Approach to Extending the Consumer Health Vocabulary. J Date Inf Sci 6(1): 35-49.
- Kirby ER, Kenny KE, Broom AF, Oliffe JL, Lewis S, et al. (2020) Responses to a Cancer Diagnosis: A Qualitative patient-centred interview study. Support Care Cancer, 28: 229-238.
- Butow PN, Kazemi JN, Beeney LJ, Griffin AM, Dunn SM, et al. (1996) When the Diagnosis is Caner. Cancer 77(12): 2630-2637.
- Back AL, Arnold RM, Baile WF, Tulsky JA, Fryer-Edwards K (2005) Approaching Difficult Communication Tasks in Oncology. CA Cancer J Clin 55: 164-177.
- OSF Healthcare Jump Simulation (2018) Applications.
- Duhn L, Medves J (2018) A 5-facet framework to describe patient engagement in patient safety. Health Expectations 21(6): 1122–1133.
-
Margaret Czart* and Dick Lui. Consumer Health Informatics for Cancer Treatment Engagement. Adv Can Res & Clinical Imag. 3(5): 2023. ACRCI.MS.ID.000575.
-
Consumer Health Informatics, Patient Engagement. Health Literacy, Digital Literacy
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
- Abstract
- Introduction
- Defining the Role of Consumer Health Informatics Professionals
- Consumer Health Engagement Frameworks Applied to Cancer
- Technology Tools
- Effective Patient Engagement
- Effective Consumer Engagement
- Health Technology Limitations for the Cancer Consumer/Patient Model
- Conclusion
- Acknowledgement
- Conflict of Interest
- References






