 Editorial
Editorial
Nutritional Management in Head and Neck Squamous Cell Cancer Patients: Unmet Medical Need in Italian Real World
Raffaele addeo1 and Michele Caraglia2*
1Oncology Unit, ASLNapoli2NORD, Frattamaggiore (Na), Italy
2Department of Precision Medicine, University of Campania, Italy
Michele Caraglia, Prof Michele Caraglia, MD, PHD, Full Professor of Biochemistry, Department of Precision Medicine, University of Campania “L. Vanvitelli”, Via L. De Crecchio, 7, 80138 Naples, Italy
Received Date:November 20, 2023; Published Date:December 11, 2023
Editorial
Head and Neck Squamous Cell Cancer (HNSCC) includes cancer of the oral cavity, oropharynx, hypopharynx and larynx and represents the seventh most common cancer worldwide with an annual incidence of approximately 700 000 [1]. Much weaker risk factors include tobacco use and alcohol consumption, and Human Papillomavirus (HPV) infection causes of oropharyngeal cancer. These tumors are frequently burdened by a diagnostic delay with approximately half of cases diagnosed in advanced stage cancer. Many patients in this setting are malnourished on diagnosis. Generally, half of all cancer patients lose some body weight; a third lose more than 5% of their original body weight and about 20% of all cancer deaths are caused directly by cachexia (through immobility, heart/respiratory failure). Specifically, HNSCC patients frequently complain several treatment-related problems such as dysphagia, mucositis, vomiting and nausea. These conditions determine reduced food intake and inevitable weight loss with simultaneous malnutrition and disnutrition. About 50% of HNSCC have malnutrition before starting radiotherapy [2]. This percentage inevitably rises during chemo-radiotherapy treatments, endangering both treatment completion and patient survival [3]. Malnutrition determines increased mortality rates as 10–20% of deaths in cancer patients can be attributed to malnutrition independently from malignancy itself [4]. It is recognized that malnutrition causes a wide range of physiological and clinically relevant complications including treatment interruption of chemo(radio) therapy, lower chemotherapy response rates that Determine Impaired Quality of Life (QoL) and increased mortality.
The incidence of weight loss at the time of diagnosis varies greatly depending on the site of the tumor.
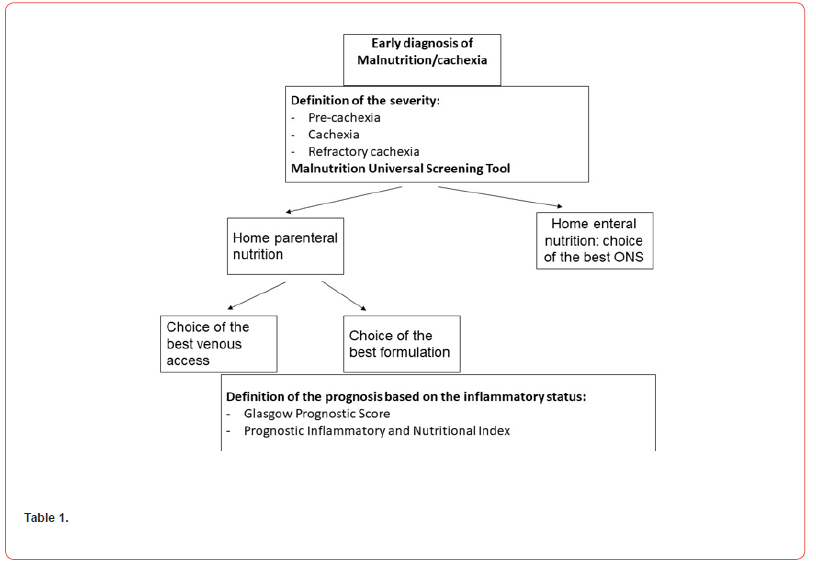
Today we have several therapeutic opportunities to overcome this important and frequent issue which further complicates the treatment of HNSCC patients. These interventions include dietary counseling or advice, oral nutritional supplements (ONS), and enteral nutrition. These weapons have induced positive effects in malnourished hospitalized and community-dwelling adults with cancer [5]. In fact, they are useful to increase dietary intake and to prevent therapy-associated weight loss and interruption of radiation therapy. Several data underline the importance of early and proactive management of malnutrition that causes a substantial improvement in clinical outcomes and QoL [6]. While almost all the oncologists were aware of the nutritional–metabolic problems that a cancer patient could experience and of the importance of adequate nutrition during treatment, the role of these interventions is still not adequate in clinical practice for different reasons and barriers. We have acquired the awareness of the importance and need for a multidisciplinary team approach for the care of these patients. However, even today there is no contribution from nutrition specialists. Many cancer centers lack an organized management to optimize the treatment of malnutrition with the aim to start nutritional treatments to the early stage of the disease. Even today there is a lot of confusion about who and how should carry out early nutritional counseling. A survey performed on a sample of 300 Italian hospital medical oncologists revealed that more than half of participants work in hospital centers where a nutritional team is absent, and, when present, composed mainly by a nutritionist (38%) or by a nutritionist and a dietician (28%) [7]. Frequently, this role is carried out by biologists who represent a valid support in the screening phase but who are not aware about the correct nutritional intervention that requires a specific medical training. Several decisions must be made before administering a nutritional support to HNSCC patients. In fact, utilizing home artificial nutrition (HAN) proves to be a suitable nutritional intervention for averting cachexia/malnutrition-related mortality and enhancing overall quality of life. Furthermore, it can seamlessly be incorporated into a home palliative care regimen. The first decision to be made is to initiate either home enteral nutrition (HEN) or home parenteral nutrition (HPN) depending upon individual patient indications and contraindications. Regarding HPN, the selection of the optimal venous access is relevant for the success of the approach. In the last 20 years, the number of central venous catheters for HPN, especially peripherally inserted central catheters, doubled [8]. In the case of HEN, the choice of the ONS (oral nutritional supplement) to be administered to the patients is often strictly dependent from their availability at the hospital pharmacy. Thus, ONS formulations are heterogeneous and vary from a cancer center to another. Moreover, their prescription is often performed by surgeons and sometimes by nutritionists or anesthesiologists, but rarely by oncologists. These discrepancies in the choice of the ONS formulation clearly impact the quality of patient care. On these bases, some corrective measures are required. It is critical to adopt strategies for an early assessment of the nutritional status in cancer patients prompting a rapid intervention with different therapeutic options. It is also critical to measure the grade and intensity of malnutrition and cachexia. In fact, it goes from pre-cachexia (malnutrition) to initial cachexia and cachexia. The definition of the severity of cachexia is based upon consolidated scores such as MUST (Malnutrition Universal Screening Tool) and the cachexiainduced inflammation is weighted through Glasgow Prognostic Score (GPS) and Prognostic Inflammatory and Nutritional Index (PNII) [9,10]. The latter are based on the evaluation of biochemical markers predictive of inflammation and bad prognosis. Moreover, an integrated network among oncologists and nutritionists is required together with the definition of guidelines for the optimal management of malnutrition/cachexia. Therefore, it is necessary an implementation of educational activities, new pathways and algorithms to design integrated teams between nutritionists and oncologists, but above all a standardization of the processes to optimize the malnutrition/cachexia management in patients with HNSCC (Table 1).
Table 1:
References
- Bray F, Ferlay J, Soerjomataram I, et al. (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6): 394-424.
- Langius JAE, Doornaert P, Spreeuwenberg MD, Langendijk JA, Leemans CR, et al. (2010) Radiotherapy on the neck nodes predicts severe weight loss in patients with early-stage laryngeal cancer. Radiother Oncol 97: 80e5.
- Unsal D, Mentes B, Akmansu M, Uner A, Oguz M, et al. (2006) Evaluation of nutritional status in cancer patients receiving radiotherapy: a prospective study. Am J Clin Oncol 29: 183e8.
- Pressoir M, Desné, S, Berchery D, Rossignol G, Poiree B, et al. (2010) Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer 102: 966-971.
- Baldwin C, Spiro A, Ahern R, Emery PW (2012) Oral nutritional interventions in malnourished patients with cancer: A systematic review and meta-analysis. J Natl Cancer ins 104: 371-385.
- Bossola M (2015) Nutritional interventions in head and neck cancer patients undergoing chemoradiotherapy: a narrative review. Nutrients 7(1): 265-276.
- Muscaritoli M, Corsaro E, Molfino A (2021) Awareness of Cancer-Related Malnutrition and Its Management: Analysis of the Results from a Survey Conducted Among Medical Oncologists. Front Oncol 682999.
- Ruggeri E, Giannantonio M, Ostan R, Agostini F, Sasdelli AS (2021) Choice of access route for artificial nutrition in cancer patients: 30 y of activity in a home palliative care setting. Nutrition 90: 111264.
- Forrest LM, McMillan DC, McArdle CS, Angerson WJ, Dagg K, (2005) A prospective longitudinal study of performance status, an inflammation-based score (GPS) and survival in patients with inoperable non-small-cell lung cancer. Br J Cancer 92(10): 1834-1836.
- Nelson KA, Walsh D (2002) The cancer anorexia-cachexia syndrome: a survey of the Prognostic Inflammatory and Nutritional Index (PINI) in advanced disease. J Pain Symptom Manage 24(4): 424-428.
-
Raffaele addeo and Michele Caraglia*. Nutritional Management in Head and Neck Squamous Cell Cancer Patients: Unmet Medical Need in Italian Real World. Adv Can Res & Clinical Imag. 4(2): 2023. ACRCI.MS.ID.000582.
-
Head and Neck Squamous Cell Cancer, Human Papillomavirus, Oropharyngeal Cancer, Determine Impaired Quality of Life
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






