 Case Report
Case Report
Superior Vena Cava Syndrome secondary to Migratory Thrombophlebitis: A Rare Complication of Behçet’s Disease
Muhammad Maaz bin Zahid1sup>, Muhammad Luqman1sup>, Muhammad Yasir2sup>, Muhammad Haris Khan1sup>, Muhammad Ijaz Khan3sup>*, Fasih Ullah Khan4sup> and Samra Israr5sup>
1Department of Medicine, Khyber Medical College, Peshawar, Pakistan
2District Headquarter Hospital, Karak, Pakistan
3MD, MBBS, MRCPI, Greater Baltimore Medical Center, Towson, MD, USA
4MBBS, Department of Medicine, Medical Teaching Institute, Gomal Medical College, Dera Ismail Khan, Pakistan
5MBBS, Khyber Medical College, Peshawar, Pakistan
Muhammad Ijaz Khan, M.D, MBBS, MRCPI, Greater Baltimore Medical Center, Towson, MD, USA
Received Date: November 01, 2024; Published Date: November 08, 2024
Abstract
Behcet’s syndrome is a multi-system chronic inflammatory condition that affects different organs. Vascular thrombosis is a common finding in this condition and constitutes its diagnostic criterion. Its involvement of superior vena cava is rather scarce with only a few cases reported in the literature. We present an 18-year-old schoolboy who presented with 1 week of low-grade fever followed by increased swelling of the neck and face. Physical examination showed bilateral neck swelling, facial swelling, and dilated veins in the neck, and the upper chest. Based on the patient’s calculation studies, a potential diagnosis of superior vena cava (SVC) obstruction due to a hypercoagulable state was considered. Two years later, the patient developed recurrent oral and genital ulcers, bilateral lower extremity weakness, diminished reflexes, loss of sensation and bladder control. After going through necessary testing Behçet’s disease (BD) was ultimately diagnosed. He was treated with anticoagulants, steroids, azathioprine, plus specific immune regimens for neurological complications and went into remission.
Keywords: Behcet’s disease; svc syndrome; vascular thrombosis; immunomodulation therapy
Introduction
Behçet’s disease (BD) is a chronic, systemic vasculitis characterized by a triad of recurrent aphthous ulcers (mouth sores), genital ulcers, and ocular symptoms [1]. While these are the cornerstone manifestations, BD can affect various organ systems. A rare but potentially life-threatening complication of BD is superior vena cava (SVC) syndrome [2]. We present a case report of a young patient with established BD who developed migratory thrombophlebitis, involving multiple veins, leading to SVC syndrome as a rare but serious complication. We discuss the clinical picture, diagnostic workup, management strategies employed, and the importance of considering SVC syndrome in the differential diagnosis of patients with BD, particularly those presenting with atypical features.
Case Presentation
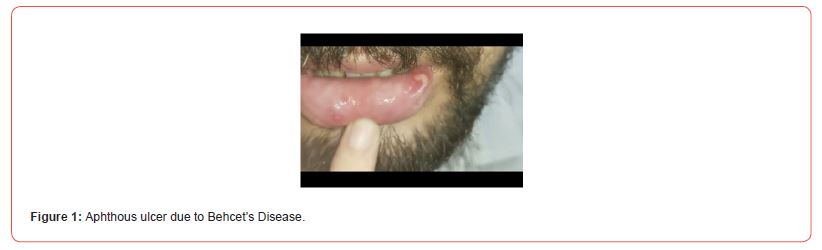
An 18-year-old school boy with no significant medical history presented to the clinic with a 1-week history of fever, and bilateral facial and neck swelling. He was a lifetime non-smoker and a nonalcoholic. He had no personal or family history of coagulopathies or cancer. There was no history of surgical or medical interventions to his neck or limbs. On physical examination, his vitals were stable. He had diffused facial and bilateral neck swelling, and several distended veins in the neck and upper chest region. Considering the results of the coagulation studies and the age of the patient, a case of SVC due to a hypercoagulable state was suspected. Anticoagulation therapy was started at that time, which led to just temporary relief, before a relapse. Two years later, he had recurrence of the same symptoms, but this time associated with recurrent genital ulcers, arthralgias, bilateral lower extremity weakness, areflexia, anesthesia, and urinary incontinence (Figure 1). On diving deep, it was disclosed that the patient has had recurrent ulcers for the past four years and were passed on for benign aphthous ulcers. They were only highlighted when the patient had already developed nervous system involvement. A possible diagnosis of SVC syndrome secondary to BD was considered.
Investigations
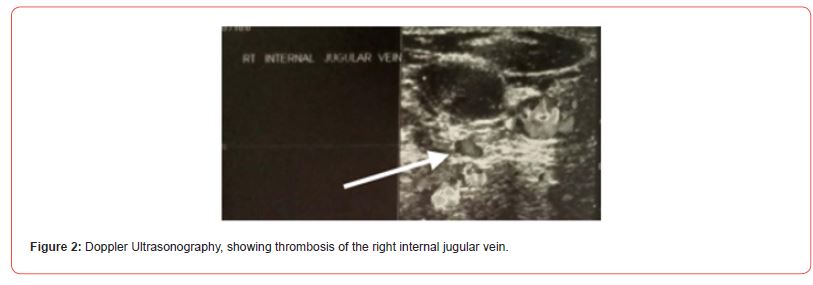
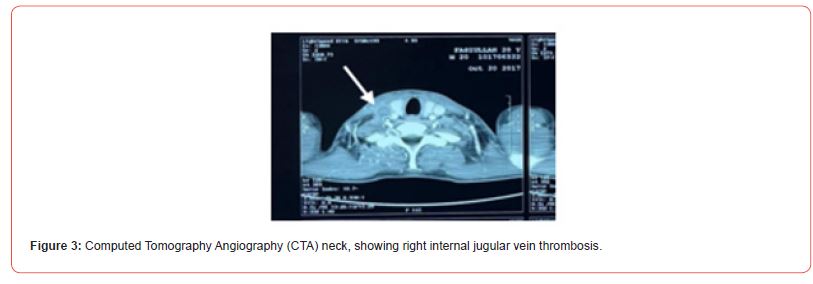
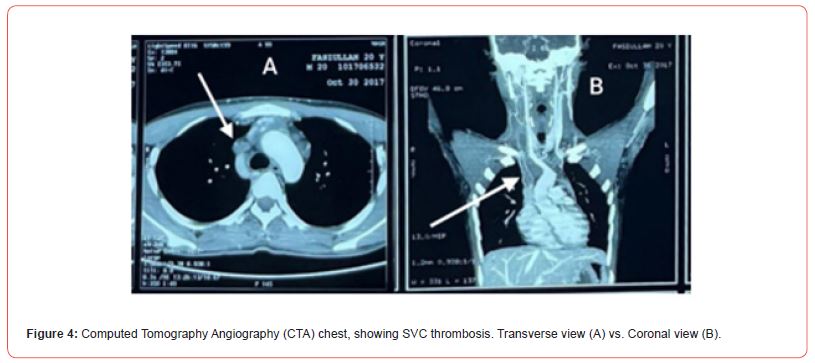
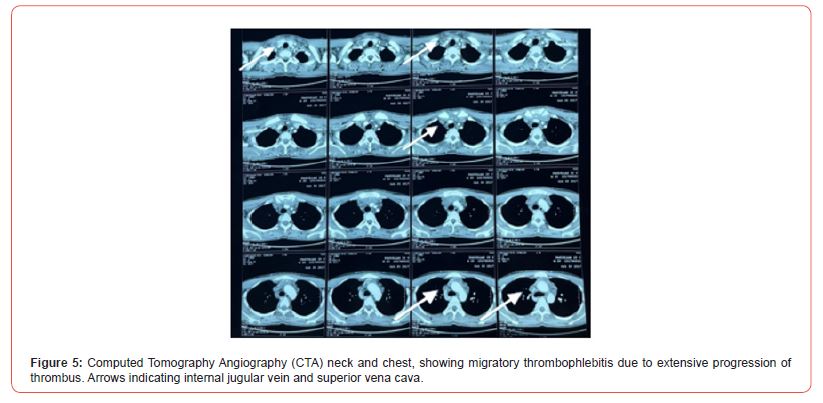
Laboratory data revealed normal hemoglobin of 14.91 g/ dL, leukocytosis at 19,860/mm3 predominantly neutrophils (83%) with an absolute neutrophil count of 16.48 x 109. He had a prolonged Prothrombin time (PT) of 23 sec with an International normalized ratio (INR) of 1.8. He also had low Protein S at 68% and weakly positive Lupus anticoagulant antibodies with an LA1/LA2 ratio of 1.4. Antinuclear antibody, immunofluorescent antibody, and anti-dsDNA were negative. The patient had a high C reactive protein (CRP), a high sensitivity of 164.24 mg/dL, and an elevated erythrocyte sedimentation rate (ESR) of 105 mm/h. Based on these findings, possible thrombosis due to a hypercoagulable state was presumed. Further investigations including Doppler ultrasonography revealed thrombosis of the right internal jugular vein (Figure 2). Computed Tomography Angiography (CTA) of the chest and neck showed right internal jugular vein thrombosis (Figure 3), extending down to involve the brachiocephalic vein and SVC (Figures 4&5). Regression of thrombus on CTA in association with vasculitis established the diagnosis of migratory thrombophlebitis.
Differential Diagnosis
Clinical presentation of SVC obstruction along with the abnormal coagulation studies led to the initial assumption of SVC syndrome due to a hypercoagulable state. However, based on the clinical picture and laboratory values, SVC syndrome from migratory thrombophlebitis due to BD was made.
Treatment
The choice of treatment was based on immunosuppression therapy to treat BD. Treatment included high-dose corticosteroids, including a 5-day pulse of methylprednisolone (1000 mg/day), and continuous prednisone 60 mg/day along with azathioprine (1000 mg/month). For SVC, anticoagulation therapy was sustained for 6 months.
Outcome and Follow-Up
The patient had an uneventful recovery after the initiation of therapy; the edema of the neck and face resolved, and the labs gradually trended down. Imaging showed a clearing of veins. The patient made a smooth transition to regular life.
Discussion
Behcet’s disease (BD) is a multisystem systemic inflammatory condition having a relapsing and remitting course. It mainly presents with mucocutaneous, ocular, and GI symptoms. However, the involvement of skin, urogenital, neurological, and vascular systems can also occur [3]. Vascular involvement in BD is rare. A respective study including 5970 patients revealed vascular involvement in 14.7% of cases [4]. Venous involvement is way more common than the arterial system, with literature showing so in up to 10-25% of cases [5]. Deep vein thrombosis (DVT) is the most common vascular presentation in patients with BD, present in 75% of the cases. It most commonly affects the femoral and the popliteal veins [6]. However, our patient hadn’t had DVTs. Vena cava thrombosis is the second most common venous malformation in patients with BD. Around 15% of the patients with BD develop vena cava thrombosis, leading to SVC syndrome [6]. The SVC is a major vein responsible for draining blood from the head, neck, upper extremities, and chest into the heart. Obstruction of the SVC presents with a constellation of symptoms due to impaired venous drainage. These symptoms can include facial and neck swelling, headache, dizziness, upper body plethora (redness), and dyspnea (difficulty breathing) [7].
The most common causes of SVC syndrome include malignancies (lymphoma, lung cancers) [8], and venous catheterization [9]. However, our patient had no history of cancer or venous catheterization. Treatment of vascular thrombosis in patients with BD is not well understood. Treatment is targeted to improve the condition of the patient and prevent relapses. Immunomodulation, along with oral glucocorticoids are the firstline agents [10]. In many cases, anticoagulation therapy is also considered. Using anticoagulation therapy to resolve the clot in patients with vascular BD is a debatable subject among physicians. Several studies state that using Heparin or Warfarin can cause serious bleeding and immense inflammation in some of these patients [11,12]. In the modern era, there is increasing evidence for the role of biologics in the treatment of BD. Drugs like canakinumab, tocilizumab, gevokizumab, and anakinra are used not only to cure the neurological manifestations of BD but have also shown benefits in vascular lesions as well [13].
Conclusion
Superior vena cava thrombosis may be seen because of thrombophlebitis during Behcet’s disease. Although Behcet’s disease is rarely considered during the investigation of SVC syndrome, it should be regarded during the search for the etiology of venous thrombosis in young and middle-aged patients without a history of cancer or coagulopathy.
References
- Erkan Alpsoy (2016) Behçet’s disease: A comprehensive review with a focus on epidemiology, etiology and clinical features, and management of mucocutaneous lesions. J Dermatol 43(6): 620-632.
- Han DS, Kim JB, Lee OY, Sohn JH, Park KN, et al. (1998) A Case of Behcet`s Syndrome with Supeior Vena Cava Syndrome. Korean J Intern Med 13(1): 72-75.
- Uyaroglu OA, Erden A, Kilic L, Peynircioğlu B, Karadag O, et al. (2019) Behçet’s disease; A rare refractory patient with vena cava superior syndrome treated with infliximab: a case report and review of the literature. Acta Clin Belg 74(5): 364-369.
- Tascilar K, Melikoglu M, Ugurlu S, Sut N, Caglar E, et al. (2014) Vascular involvement in Behçet’s syndrome: a retrospective analysis of associations and the time course. Rheumatology 53(11): 2018-2022.
- Fei Y, Li X, Lin S, Song X, Wu Q, et al. (2013) Major vascular involvement in Behçet’s disease: a retrospective study of 796 patients. Clin Rheumatol 32(6): 845-852.
- Demirtürk OS, Tünel HA, Alemdaroğlu U (2017) Vascular Manifestations of Behçet’s Disease. Gonul M, Kartal SP, [Eds.,]. Behcet’s Disease.
- Seligson MT, Surowiec SM (2024) Superior Vena Cava Syndrome. Treasure Island (FL): StatPearls Publishing.
- Wing SC, Ricketts WM, Banka RB, Nagy Z, Ellis S (2012). A rare cause for superior vena cava obstruction. BMJ Case Rep 2012006456.
- Morriello F, Brown A, Granton J, Bonta M (2023) Catheter-associated superior vena cava syndrome. CMAJ 195(2): E72-E75.
- Radke PW, Schwarz ER, Groesdonk H, Graf J, Janssens U(2001) J Thromb Thrombolysis 11(2): 137-141.
- Ouchi K, Narui R, Sakuma T, Ojiri H (2020) Serious Complication of Anticoagulation in Vessel Thrombosis- associated Behçet Disease. Intern Med 59(13): 1615-1620.
- Desbois AC, Wechsler B, Resche‐Rigon M, Piette JC, Huong DLT, et al. (2012) Immunosuppressants reduce venous thrombosis relapse in Behçet’s disease. Arthritis Rheum 64(8): 2753-2760.
- Caso F, Costa L, Rigante D, Lucherini OM, Caso P, et al. (2014) Biological Treatments in Behçet’s Disease: Beyond Anti-TNF Therapy. Mediators Inflamm 2014: 107421.
-
Muhammad Maaz bin Zahid, Muhammad Luqman, Muhammad Yasir, Muhammad Haris Khan, Muhammad Ijaz Khan*, Fasih Ullah Khan and Samra Israr. Superior Vena Cava Syndrome secondary to Migratory Thrombophlebitis: A Rare Complication of Behçet’s Disease. Arch Clin Case Stud. 4(3): 2024. ACCS.MS.ID.000587.
-
Disulfidptosis; breast cancer; subtypes; prognosis model; ceRNA; iris publishers; iris publisher’s group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






