 Case Report
Case Report
Ruptured Solid Pseudopapillary Tumor of Pancreas Presented as an Acute Abdomen: A Case Report
Tafese Gudissa Merga1*, Hana Abebe Gebreselassie1, Hawi Debebe Fura2 and Maru Gama Erge1
1Saint Paul’s Hospital Millennium Medical College, Department of Surgery, Addis Ababa, Ethiopia
2Saint Paul’s Hospital Millennium Medical College, Department of Pathology, Addis Ababa, Ethiopia
Tafese Gudissa Merga, Saint Paul’s Hospital Millennium Medical College, Department of Surgery, Addis Ababa, Ethiopia
Received Date: September 06, 2024; Published Date: September 13, 2024
Abstract
Background: A solid pseudopapillary tumor of the pancreas is one of the rare pancreatic tumors. It usually occurs in young women. The common clinical presentation of this tumor is nonspecific abdominal pain and abdominal mass. Since it has low malignancy potential, with complete surgical resection, the outcome is excellent.
Case presentation: We report the case of a 12-year-old female who presented with hemorrhagic shock secondary to bleeding from a ruptured pancreatic head mass after she sustained blunt abdominal trauma. The patient underwent surgery, and a mass excision was done. She had a smooth postoperative course and was discharged on six postoperative days. The biopsy revealed a solid pseudopapillary tumor.
Clinical discussion: A solid pseudopapillary tumor is a rare tumor arising from the pancreas. It usually presents with nonspecific symptoms including abdominal pain and mass. It may also present with features of obstructive jaundice and gastric outlet obstruction. Presentation with acute abdomen due to tumor rupture is an extremely infrequent presentation. Imaging and histopathologic evaluation play a great role in the diagnosis of this disease. The disease is known for its benign nature with excellent outcomes after surgical excision.
Conclusion: Even though solid pseudopapillary tumor is a rare occurrence in the pediatric age group, it should be considered in female adolescents who present with pancreatic mass. Complete surgical resection suffices for the treatment.
Keywords: Solid pseudopappilary tumor; pancreas; acute abdomen; pediatrics
Introduction
Solid pseudopapillary tumor (SPPT) is a rare tumor arising from the pancreas [1,2]. It usually occurs in young female patients. Its presentation is usually nonspecific symptoms including abdominal pain and gradually increasing abdominal mass. Some patients can present with nausea, vomiting, and jaundice. Very rarely spontaneous tumor rupture can be the initial patient presentation. The diagnosis of SPPT depends on clinical presentation, imaging, and pathologic evaluation. Imaging and histopathology play a great role. It is known for its benign nature with excellent outcomes after surgical intervention, but about 10% of these tumors are malignant with possible local invasion and distal metastasis [3,4]. We are reporting a pediatric patient who was presented with hemorrhagic shock from a bleeding solid pseudopapillary tumor after sustaining blunt abdominal trauma and managed in a resource- limited area.
Case Presentation
A 12-year-old female presented to a primary hospital with the complaint of abdominal pain after she sustained blunt abdominal trauma 5 hours before presentation. Upon arrival at the hospital, she was in shock. After assessing her, it was determined that she was experiencing hemorrhagic shock due to intrabdominal bleeding caused by a solid organ injury. She was resuscitated with crystalloids, and an exploratory laparotomy was performed. The intraoperative finding was about 2 liters of intraperitoneal hemorrhage along with a bleeding mass located between the duodenum (first and second part) and the pancreatic head. Omental buttressing was done to control the bleeding. However, due to a lack of blood products for transfusion and the difficulty of dealing with the mass, she was referred to our hospital. At the presentation to our hospital, after about 36 hours of the trauma, she was tachycardic (Pulse rate of 140), tachypneic (respiratory rate of 28), and febrile (temperature of 38.6oC), but blood pressure (blood pressure of 100/60mmHg) was within the normal limit and had adequate urine output. She was fully conscious. She had pale conjunctiva and palmar pallor.
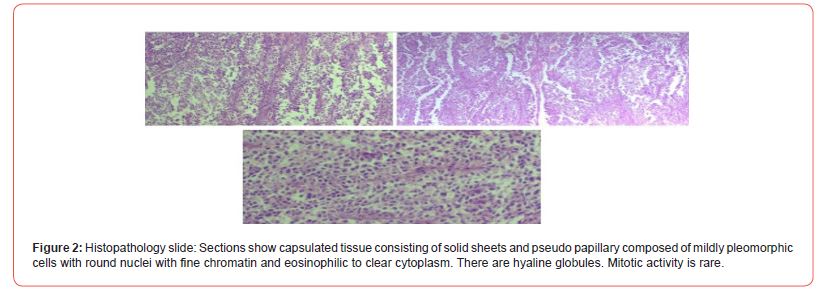
There was diffusing tenderness whole over the abdomen with positive signs of fluid collection. Complete blood count was determined, and hemoglobin was 3 gm/dl with a hematocrit of 9%. She was transfused with 2 units of packed red blood cells and taken to the operating room. Since the patient was having a future of generalized peritonitis with positive signs of fluid collection on physical examination, she didn’t undergo any imaging modalities. The intraoperative finding was about 300 ml of hemorrhagic fluid in the general peritoneum. There was a mass that measured about 6cm * 8cm with a firm and smooth surface which was located between the duodenum and the pancreas. It was attached to the pancreatic head and adherent to the duodenal wall (first and second part). The mass was enucleated out (Figures 1&2). But during removal, there was an iatrogenic duodenal perforation which was primarily repaired, since the tissue was not fragile it was repaired without patching. There was no injury to pancreatic ducts. There was no local invasion, no lymphadenopathy, and no liver metastasis seen. The mass was sent for histopathologic evaluation which revealed a solid pseudopancreatic tumor (Figure 2). The patient was discharged on six postoperative days and she is having a smooth postoperative course at 1-year postoperative follow-up (Figures 1&2).

Discussion
Solid pseudopapillary tumors of the pancreas are one of the rare tumors arising from the pancreas. It commonly arises from the tail and body of the pancreas but in the pediatric age group, the pancreatic head is the most common site as in our patient [5- 7]. This tumor is predominantly seen in young females with a peak age of 20-30 years but can affect any age [7-10]. It is characterized by a benign nature. However, about 10% of solid pseudo-papillary tumors are malignant and there may be local invasion and distal metastasis to the liver and the lung at the time of diagnosis. Tumors with larger size and occurring at extreme ages, less than 10 years and above 50 years, are associated with more malignancy potential [4,11-16]. Patients with solid pseudopapillary tumors usually present with nonspecific abdominal symptoms. The most common presentation is gradually progressive abdominal mass and abdominal pain, but nausea, vomiting, and jaundice can be the initial presentation rarely with spontaneous tumor rupture [7,17- 21].
Imaging plays a role in the diagnosis of SPPT. On a multiphasic CT scan the tumor is characterized by cystic and solid components showing weak early arterial enhancement compared to normal parenchyma and the solid component shows a gradual increase in enhancement in the portal-venous phase, exceeding the normal parenchyma [22,23]. The correct diagnosis of SPPT depends on careful analysis of clinical features, imaging findings, and histopathologic evaluation [24-27]. Complete resection of the tumor is the main goal of treatment of SPPT. Even patients with malignant SPPT have excellent prognosis with complete resection of the tumor [12,28-31]. The type of surgery performed will depend on the anatomic location of the tumor and the extent of the tumor. The possible procedures performed are tumor enucleation, partial pancreatectomy, or pancreaticoduodenectomy depending on the site, extent, and nature of the tumor [7,24,26,29,32].
Conclusion
We report a rare case of a solid pseudopapillary tumor of the pancreas in a 12-year-old female child who presented with hemorrhagic shock from a ruptured solid pseudopapillary tumor following blunt abdominal trauma. Even though pancreatic tumors are uncommon in pediatrics, the possibility of SPPT should be kept in mind for patients presented with bleeding pancreatic masses.
Declarations
Ethics approval and consent to participate
Both ethical clearance and consent to participate were approved by the institutional review board for this case report.
Consent for publication
Ethical approval is held to be unnecessary by St. Paul’s Hospital Millennium Medical College Institutional Review Board as this is a single rare case encountered during clinical practice.
Availability of supporting data
All data and materials are available upon request by the Editorin- Chief.
Competing interests
No authors have disclosed any conflicts of interest.
Funding
Not applicable.
Authors’ contributions
All authors contributed in different aspects. EM and GA operated on the patient and also following the patient. FH reviewed the histopathologic slide. MT operated on the patient, wrote the case report and is also following the patient. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank the patient’s guardians for giving us consent to use both the child’s history and the different pictures.
References
- Speer AL, Barthel ER, Patel MM, Grikscheit TC (2012) Solid pseudopapillary tumor of the pancreas: A single-institution 20-year series of pediatric patients. J Pediatr Surg 47(6): 1217-12122.
- Francis WP, Goldenberg E, Adsay NV, Steffes CP, Webber JD (2006) Solid-Pseudopapillary Tumors of the Pancreas: Case Report and Literature Review. Curr Surg 63(6): 469-472.
- Seung Hoon Choi, Seong Min Kim, Jung Tak Oh, Jin Young Park, Jeong Meen Seo, et al. (2006) Solid pseudopapillary tumor of the pancreas: a multicenter study of 23 pediatric cases. J Pediatr Surg 41(12): 1992-1995.
- Adams AL, Siegal GP, Jhala NC (2008) Solid Pseudopapillary Tumor of the Pancreas A Review of Salient Clinical and Pathologic Features. Adv Anat Pathol 15(1): 39-45.
- Seung Eun Lee, Jin-Young Jang, Dae Wook Hwang, Kwi-Won Park, Sun-Whe Kim (2008) Clinical Features and Outcome of Solid Pseudopapillary Neoplasm Differences Between Adults and Arch Surg 143(12): 1218-1221.
- Ning Guo, Quan B Zhou, Ru F Chen, Sheng Q Zou, Zhi H Li, et (2011) Diagnosis and surgical treatment of solid pseudopapillary neoplasm of the pancreas: Analysis of 24 cases. Can J Surg 54(6): 368-374.
- Feng Yang, Chen Jin, Jiang Long, Xian Jun Yu, Jin Xu, et al. (2009) Solid pseudopapillary tumor of the pancreas: a case series of 26 consecutive patients. Am J Surg 198(2): 210-215.
- Cheng-hong Peng, Dong-feng Chen, Guang-wen Zhou, Wei-ping Yang, Zong-yuan Tao, et (2006) The solid-pseudopapillary tumor of the pancreas: the clinical characteristics and surgical treatment. J Surg Res 131(2): 276-282.
- Peng-Fei Yu, Zhen-Hua Hu, Xin-Bao Wang, Jian-Min Guo, Xiang-Dong Cheng, et (2010) Solid pseudopapillary tumor of the pancreas: A review of 553 cases in Chinese literature. World J Gastroenterol 16(10): 1209-1214.
- Ghita Berrada, Soukaina Belaaroussi, Kamilia Chbani, Siham Salam, Dalal Laoudiyi, et al. (2020) Solid pseudopapillary tumor of the pancreas: A rare entity in Pan Afr Med J 35: 137.
- Jin-Young Choi, Myeong-Jin Kim, Joo Hee Kim, Seung Hyoung Kim, Joon Sok Lim, et al. (2006) Solid pseudopapillary tumor of the pancreas: typical and atypical manifestations. AJR Am J Roentgenol 187(2): W178-W186.
- Song H, Dong M, Zhou J, Sheng W, Zhong B, et al. (2017) Solid Pseudopapillary Neoplasm of the Pancreas: Clinicopathologic Feature, Risk Factors of Malignancy, and Survival Analysis of 53 Cases from a Single Center. Biomed Res Int 2017: 5465261.
- Kim CW, Han DJ, Kim J, Kim YH, Park JB, et al. (2011) Solid pseudopapillary tumor of the pancreas: Can malignancy be predicted? Surgery 149(5): 625-634.
- Moo Kang C, Sik Kim K, Sub Choi J, Kim H, Jung Lee W, et al. (2006) Solid Pseudopapillary Tumor of the Pancreas Suggesting Malignant Potential. Pancreas 32(3): 276-280.
- Hwang J, Kim DY, Kim SC, Namgoong JM, Hong SM (2014) Solid-pseudopapillary neoplasm of the pancreas in children: Can we predict malignancy? J Pediatr Surg 49(12): 1730-1733.
- Laje P, Bhatti TR, Adzick NS (2013) Solid pseudopapillary neoplasm of the pancreas in children: A 15- year experience and the identification of a unique immunohistochemical marker. J Pediatr Surg 48(10): 2054-2060.
- Nguyen NQ, Johns AL, Gill AJ, Ring N, Chang DK, et al. (2011) Clinical and immunohistochemical features of 34 solid pseudopapillary tumors of the J Gastroenterol Hepatol 26(2): 267-274.
- Bender AM, Thompson ED, Hackam DJ, Cameron JL, Rhee DS (2018) Solid pseudopapillary neoplasm of the pancreas in a young pediatric patient: A case report and systematic review of the literature. Pancreas 47(10): 1364-1368.
- Lima CA, Silva A, Alves C, Alves A, Lima S, et al. (2017) Solid pseudopapillary tumor of the pancreas: Clinical features, diagnosis and Rev Assoc Med Bras 63(3): 219-223.
- Rebhandl W, Felberbauer FX, Puig S, Paya K, Hochschorner S, et al. (2001) Solid- Pseudopapillary Tumor of the Pancreas (Frantz tumor) in Children: Report of Four Cases and Review of the Literature. J Surg Oncol 76(4): 289-296.
- Sandesh V Parelkar, Sanjay N Oak, Satish P Kapadnis, Beejal V Sanghvi, Prashant B Joshi, et (2013) Solid pseudopapillary tumor of the pancreas: An unusual tumor in children. J Indian Assoc Pediatr Surg 18(1): 38-40.
- Qihua Yin, Mingliang Wang, Chengsheng Wang, Zhiyuan Wu, Fei Yuan, et (2012) Differentiation between benign and malignant solid pseudopapillary tumor of the pancreas by MDCT. Eur J Radiol 81(11): 3010-3018.
- Dong-Li Li, Hong-Sheng Li, Yi-Kai Xu, Quan-Shi Wang, Rui-Ying Chen, et al. (2018) Solid pseudopapillary tumor of the pancreas: clinical features and imaging findings. Clin Imaging 48: 113-121.
- László Romics, Attila Oláh, Tibor Belágyi, Nóra Hajdú, Péter Gyurus, et al. (2010) Solid pseudopapillary neoplasm of the pancreas-proposed algorithms for diagnosis and surgical treatment. Langenbecks Arch Surg 395(6): 747-755.
- Saad Al-Qahtani, Francois Gudinchet, Tarek Laswed, Pierre Schnyder, Sabine Schmidt, et al. (2010) Solid pseudopapillary tumor of the pancreas in children: typical radiological findings and pathological correlation. Clin Imaging 34(2): 152-156.
- Darshan Gandhi, Pranav Sharma, Kalind Parashar, Puneet S Kochar, Kriti Ahuja, et al. (2020) Solid pseudopapillary Tumor of the Pancreas: Radiological and surgical Clin Imaging 67: 101-107.
- Yao J, Song H (2020) A Review of Clinicopathological Characteristics and Treatment of Solid Pseudopapillary Tumor of the Pancreas with 2450 Cases in Chinese BioMed Res Int 2020:2829647.
- Sushanth Reddy, John L Cameron, Jennifer Scudiere, Ralph H Hruban, Elliot K Fishman, et (2009) Surgical Management of Solid-Pseudopapillary Neoplasms of the Pancreas (Franz or Hamoudi Tumors): A Large Single- Institutional Series. J Am Coll Surg 208(5): 950-957.
- Theodossios Papavramidis, Spiros Papavramidis (2005) Solid pseudopapillary tumors of the pancreas: Review of 718 patients reported in English literature. J Am Coll Surg200(6): 965-972.
- Jinhua Ye, Mingzhe Ma, Dongfeng Cheng, Fei Yuan, Xiaxing Deng, et (2012) Solid-pseudopapillary tumor of the pancreas: Clinical features, pathological characteristics, and origin. J Surg Oncol 106(6): 728-735.
- Ayşe Yagc, Savas Yakan, Ali Coskun, Nazif Erkan, Mehmet Yıldırım, et (2013) Diagnosis and treatment of solid pseudopapillary tumor of the pancreas: experience of one single institution from Turkey. World J Surg Oncol 11:308.
- Jean M Butte, Murray F Brennan, Mithat Gönen, Laura H Tang, Michael I D'Angelica, et (2011) Solid pseudopapillary tumors of the pancreas. clinical features, surgical outcomes, and long-term survival in 45 consecutive patients from a single center. J Gastrointest Surg 15(2): 350-357.
-
Tafese Gudissa Merga*, Hana Abebe Gebreselassie, Hawi Debebe Fura and Maru Gama Erge. Ruptured Solid Pseudopapillary Tumor of Pancreas Presented as an Acute Abdomen: A Case Report. Arch Clin Case Stud. 4(2): 2024. ACCS.MS.ID.000584.
-
Solid pseudopappilary tumor; pancreas; acute abdomen; pediatrics; iris publishers; iris publisher’s group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






