 Case Report
Case Report
Gastrointestinal Bleeding in a Full-Term Infant: A Case Report
Tijerina Tijerina Gabriela1*, Oldak Skvirsky David2, Cázares Méndez Josefina Monserrat3, Hernández Duck Elias4, Escobedo Berumen Lucia5 and Ramírez Nova Sergio6
1,4,6Department of Neonatology, Hospital Ángeles Lomas, Mexico
2Department of Neonatology, Head of the Neonatology Division at Hospital Ángeles Lomas, Mexico
3Department of Pediatric gastroenterologist and pediatric digestive endoscopist, National Institute of Pediatrics, Mexico
5Pediatric gastroenterology resident at the National Institute of Pediatrics, Mexico
Tijerina Tijerina Gabriela, Department of Neonatology, Hospital Ángeles Lomas, Mexico.
Received Date: June 27, 2020; Published Date: July 22, 2020
Abstract
A full-term newborn, during his first day of life, presented acute onset of gastrointestinal bleeding. After analyzing the case, including endoscopic evaluation and biopsy, the diagnosis of gastric and duodenal ulcers was made. The patient had conservative treatment. The bleeding and ulcers resolved over time, but the etiology remains uncertain.
Keywords:Newborn; Gastric ulcers; Gastroduodenal ulcers; Digestive bleeding; Endoscopy
Introduction
Upper gastrointestinal bleeding (UGIB) originates proximal to the Tretiz ligament, from the esophagus, stomach, and duodenum [1]. It is a potentially serious issue since it can be life-threatening. Fortunately, most of the entities that produce it do not require any surgical treatment [1]. UGIB is relatively frequent in newborns who are in an intensive care unit because it is generally associated with perinatal asphyxia, cesarean section, respiratory distress syndrome and sepsis [2,3]. However, it is rare in an apparently healthy newborn [3]. The differential diagnosis includes coagulopathies such as newborn hemorrhagic disease, cow’s milk protein allergy, sepsis, hereditary bleeding disorders, necrotizing enterocolitis, intussusception, and vascular abnormalities [3].
Another differential diagnosis is an acid-peptic disease, which is not frequent in infants. This occurs when there is an imbalance between cytotoxic and protective factors in the upper gastrointestinal tract. Cytotoxic mechanisms include excessive production of acid, pepsin, non-steroidal anti-inflammatory drugs, bile acids, and H. pylori infection [4].
Description of the Case
This is the case of a newborn female with a history of a healthy 29-year-old mother with a full-term pregnancy (38.6 gestational age), adequate prenatal control, normal structural ultrasounds and negative TORCH. She was born vaginally with clear amniotic fluid; basic resuscitation was applied. Normal physical examination: Apgar index 9/9, weight 2,630 Kg, and body length 49 cm. Intramuscular vitamin K 1mg was applied and exclusive breastfeeding began. At the end of her first day of life, she suddenly presented abundant vomiting with fresh blood. An orogastric tube was placed obtaining 15 ml of fresh blood (Figure 1). Clinically, she looked stable with good hydration and vital signs within normal limits. Soft abdomen without visceromegaly, slight pain on deep palpation, normally active peristalsis, umbilical stump without infection data.
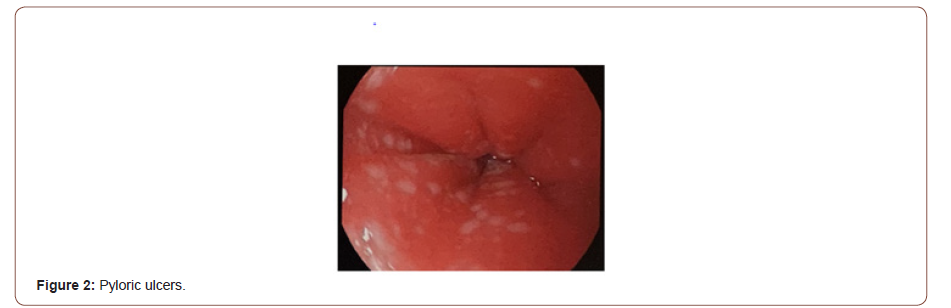
A diagnostic approach was initiated; no bleeding from maternal nipples was found. Fasting began, with required intravenous solution, omeprazole 2 mg/Kg/day, and continuous monitorization. Laboratories findings, normal hematic biometry: hemoglobin 21.1 g/dL; hematocrit 64%; leukocytes 9,000; neutrophils 70%; lymphocytes 18%; eosinophils 2%; bands 2%; platelets 134,000. TP 21.2 seconds (14.4-16.4 seconds); INR 1.7 (1.1 -1.3); TPT 33.4 seconds; blood chemistry without alterations; and no hydro electrolytic imbalance. Liver function tests and ammonia were normal. PCR for cytomegalovirus and herpes 1-2 were negative. Mother’s gastrin levels were normal (39 pg/mL). A pediatric gastroenterologist was consulted, who performed an endoscopy that reported: “multiple ulcers in the esophagus approximately 0.5cm, stomach ulcers 0.5-1cm, duodenum with a 1.5 cm ulcer” (Figures 2 & 3).

The biopsy reported “…focally ulcerated acute and chronic esophagitis, few eosinophils, edema and vascular congestion of the subepithelial stroma, mild chronic gastritis with minimal activity, no H pylori or histological data of malignancy are observed. Acute and chronic inflammation of the intestinal mucosa, no microorganisms or viral cytopathic damage is observed.” On the second day of life, she started breastfeeding again. The bleeding stopped and our patient continues with good evolution; normal stools are reported. She is discharged with oral treatment: sucralfate 80 mg/Kg/day and esomeprazole 2 mg/Kg/day. At 3 months of life, the patient is asymptomatic with adequate growth and development, exclusive breastfeeding, and without medications.
Discussion
This is a healthy, full-term newborn without any risk factor for developing ulcerative gastropathy. The endoscopic evaluation was crucial in determining the diagnosis and potential treatment. Ulcerative gastropathy is an uncommon described entity and we reported the first case in national literature. To make the diagnosis, it is important to have a complete prenatal history, as well as questioning all the maternal factors that can be related to cause of stress events. There are few reports associating gastric ulcers with psychosocial factors. However, the literature supports the concept that exposure to prenatal stress can alter the health and development of the fetus [5]. High levels of maternal gastrin have been implicated in such cases, but the transplacental passage of this hormone to the fetus is uncertain, as well as the role it plays in the development of isolated ulcers [6]. In this case, gastrin levels in the mother were normal. However, these levels were performed days after the birth of our patient. When questioning the mother, she refers to epigastric abdominal pain in almost the entire course of the pregnancy, as well as having required anti-acid drugs.
The treatment should be conservative since recurrences are rare [7]. The etiology of ulcers and UGIB will remain uncertain and it will be necessary to assess whether perinatal stress influences intestinal development, in order to identify and diagnose these patients early.
Conclusion
Ulcerative gastropathy should be a diagnosis to consider when dealing with an apparently healthy newborn who suddenly presents UGIB. Endoscopy is necessary to rule out any other pathology, in addition to biopsies. It is important to rule out maternal bleeding, infectious diseases such as cytomegalovirus and herpes 1 and 2, among others.
Acknowledgement
None.
Conflict of Interest
No Conflicts of Interest.
References
- Romano C, Oliva S, Martellossi S, Erasmo Miele, Serena Arrigo, et al. (2017) Pediatric gastrointestinal bleeding: Perspectives from the Italian Society of Pediatric Gastroenterology. World J Gastroenterol 23(8): 1328-1337.
- Joshi A, Shrestha PS, Dangol S, Shrestha NC, Poudyal P, et al. (2016) Stress induced gastric ulcers: presenting as massive rectal bleeding in a newborn. Kathmandu Univ Med J (KUMJ) 14(54): 186-189.
- Liebman WM, Thaler MM, Bujanover Y (1978) Endoscopic evaluation of upper gastrointestinal bleeding in the newborn. Am J Gastroenterol 69(5): 607-608.
- Mezoff AG, Balistreri WF (1995) Peptic ulcer disease in children. Pediatrics in review / AAP 16(7): 257-65.
- Coussons Read ME (2013) Effects of prenatal stress on pregnancy and human development: mechanisms and pathways. Obstet Med 6(2): 52-57.
- Lazzaroni M, Petrillo M, R Tornaghi, E Massironi, M Sainaghi, et al. (2002) Upper GI bleeding in healthy full-term infants: A case-control study. Am J Gastroenterol 97(1): 89-94.
- Man DW (1986) Massive upper gastrointestinal bleeding from hemorrhagic gastritis in the newborn. Aust N Z J Surg 56(11): 871-872.
-
Tijerina Tijerina G, Oldak Skvirsky D, Cázares Méndez JM, Hernández Duck E, Escobedo Berumen L, Ramírez Nova S. Gastrointestinal Bleeding in a Full-Term Infant: A Case Report. Arch Clin Case Stud. 2(4): 2020. ACCS.MS.ID.000543.
-
Dialysis Access Steal Syndrome, Ischemic monomelic neuropathy, Limb Ischemia, AV access, Peripheral vascular disease, Paresthesia, Absent pulses, Cerebrovascular disease, Hypertension.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






