 Research Article
Research Article
The Effects Of COVID-19 On Chronic Pain Patients: An Observational Survey Study
Omar Alnatour1*, Saba Javed2
1University of Texas Health Science Center at Houston, Texas, USA
2Department of Pain Medicine, University of Texas, MD Anderson Cancer Center, Houston, Texas, USA
Omar Alnatour, University of Texas Health Science Center at Houston, Texas, USA
Received Date:January 12, 2024; Published Date:January 26, 2024
Abstract
Background: The field of chronic pain faces many unique challenges in the ever-changing world that many chronic pain patients found
themselves in during the recent COVID-19 pandemic and the unpredictable years to come. Well-known now are the impacts of factors such as age,
body mass index (BMI), race, and physical activity on COVID-19 outcomes, but what impacts can these very factors have on chronic pain?
Aim: To determine if potential predictors including BMI, ethnicity, covid positivity, use of telemedicine, site of work, increase in narcotic use,
exercise level, and education level were associated with worsening of chronic pain in chronic pain patients.
Materials and Methods: This study utilized a questionnaire provided to 261 patients in an outpatient chronic pain clinic. The findings from this
questionnaire were incorporated in a univariate and multivariate logistic regression model in order to determine which, if any, potential predictors
were associated with worsening of chronic pain.
Results: To understand the joint effects of the above listed predictors, our multivariate analysis suggests that increase in chronic pain is
associated with BMI (>30), ethnicity (Caucasians less likely compared to African Americans), exercise frequency (2-4 days/week less likely), increase
narcotic use, and Covid-19 positivity.
Conclusions: Our study, the first of its kind, presents finding which suggest that worsening of chronic pain in chronic pain patients is associated
with BMI (>30), ethnicity, exercise frequency, increase in narcotic use, and covid positivity.
Keywords:BMI; chronic pain; covid-19; telemedicine; work from home; exercise
Introduction
The recent COVID-19 pandemic has impacted the world in many profound and long-lasting ways, from the immense loss of life to global economic hardship and more. As of August 2022, the World Health Organization (WHO) has documented over 550,000,000 cases and over 6,300,000 deaths across the world since the start of the pandemic [1]. It is well known that the pandemic led to a dramatic decline in the utilization of outpatient care but less recognized is the impact this pandemic has directly had on chronic pain patients in the outpatient population in regard to their chronic pain. Well-known now are the impacts of factors such as age, body mass index (BMI), race, physical activity, and social distancing on COVID-19 outcomes, but what impacts can these very factors have on chronic pain? It is well known that the pandemic led to increased utilization of telemedicine among clinics and telecommuting amongst workers, in attempts to decrease spread of the virus, but what impacts did these changes have on chronic pain? Thus, we present the first known study to look at the impacts of potential predictors including age, gender, BMI, race, use of telemedicine, work location, education level, physical activity level, marital status, and children on worsening of chronic pain in chronic pain patients.
Materials and Methods
Research Approval and Ethics Check Statement
This study was approved by our institution and survey details were disclosed to participants prior to obtaining voluntary written informed consent. Only the consenting adults were given the survey to complete. All patient identifiers were removed from the survey and all information was kept secured in a secure location. This observational survey study was conducted at an academic outpatient pain clinic from May 2020 - June 2021. The information gathered on the survey included the following information: gender, age, body mass index (BMI), race, education, marital status, work location, exercise, covid positivity, use of telemedicine during pandemic, and increase in narcotics usage during the pandemic.
Results
Statistical Methods
The primary analytic method was logistic regression in which the dependent variable was self-reported increase in chronic pain. In the first stage, we specified univariate logistic models between each of the candidate explanatory variables and dependent variable. In the second stage, we specified a multivariate logistic regression model with the set of all the candidate explanatory variables that were significant at p<0.05 (from the univariate analysis) as predictors of the dependent variable.
Participants and Design
261 patients from an outpatient chronic pain clinic participated in a survey in which they responded to questions including increase in chronic pain during the pandemic, and a set of potential predictors including covid positivity, increase in narcotic use, use of telemedicine, age category, gender, BMIOver30 (created by dichotomizing BMI), education, exercise duration, and the site of work. A sample survey is provided as shown in (Figure 1). The description of the sample and demographic data is provided in (Table 1) below. We specified a logistic regression model to assess the impact of these risk factors on the increase in chronic pain during the COVID-19 pandemic. To facilitate the estimation, some of the sparse categories were combined as follows. Education was combined to three levels, HS/Occupational (reference), College, and Graduate. Ethnicity was combined to four levels, African American (reference), Hispanic, Caucasian, and Asian/Mixed/Other. Whether the work-location was onsite or not was reduced to two levels, no (created by combining ‘Not Working’ and ‘Work from Home’) and Yes (‘On-site’).
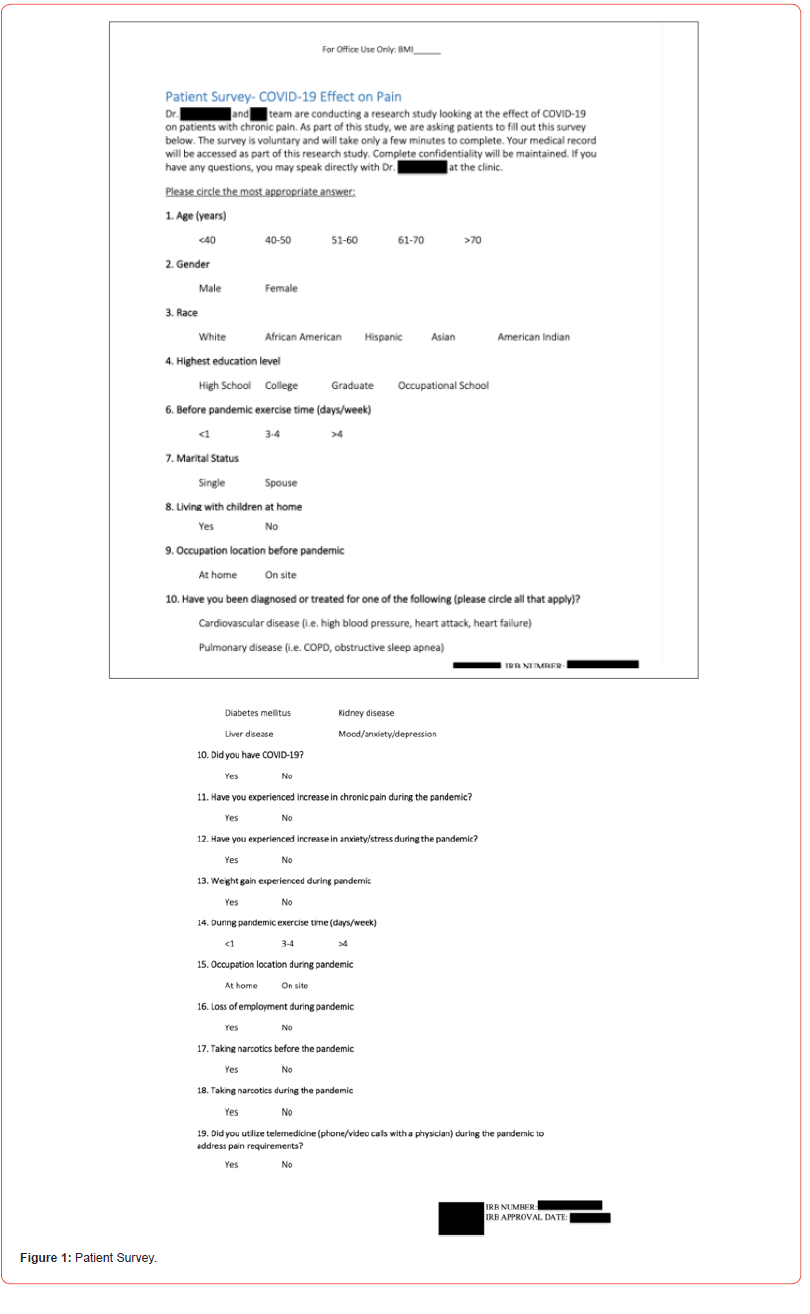
Table 1:Demographic and Situational Characteristics.
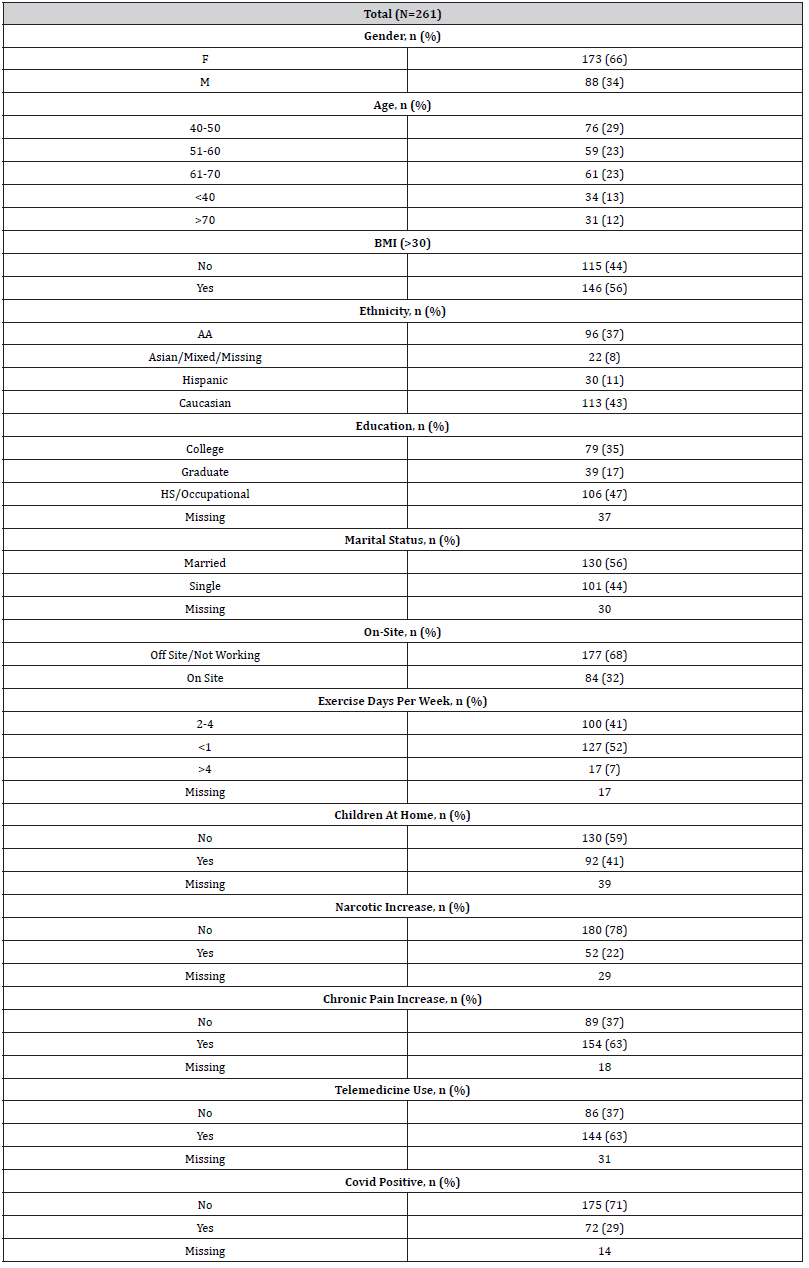
We initially specified univariate regressions in which the effect of each predictor was assessed one-at-a-time on increase in chronic pain. The results are presented in Table 2A (univariate logistic regression effects on increase in chronic pain) and Table 2B (Odds Ratio Estimates of Predictors of Increase in Chronic Pain (Univariate)) below. To assess the association between the individual predictors (Table 2A) and increase in chronic pain, we examined the p-value of the effects (Table 2A) and followed it up with an examination of the odds ratio (OR) (Table 2B), along with the confidence limits (CL). Table 2A shows the list of all univariate predictors (all categorical) that were used in the logistic regression model predicting increase in chronic pain. Among the 12 predictors gender, age, education, and marital status do not show evidence of significant association using the traditional cut-off of p<.05. Table 2B describes the strength of association between the predictor and worsening of chronic pain. For categorical predictors, the odds ratio is a measure of how the level of the predictor (relative to the reference level) is associated with change in the dependent variable (increase in chronic pain).
Table 2A:Univariate Logistic Regression Effects on Increase in Chronic Pain.
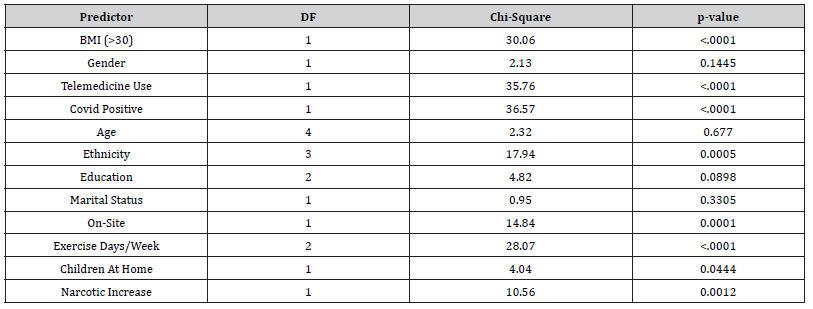
Table 2B:Odds Ratio Estimates of Predictors of Increase in Chronic Pain (Univariate).
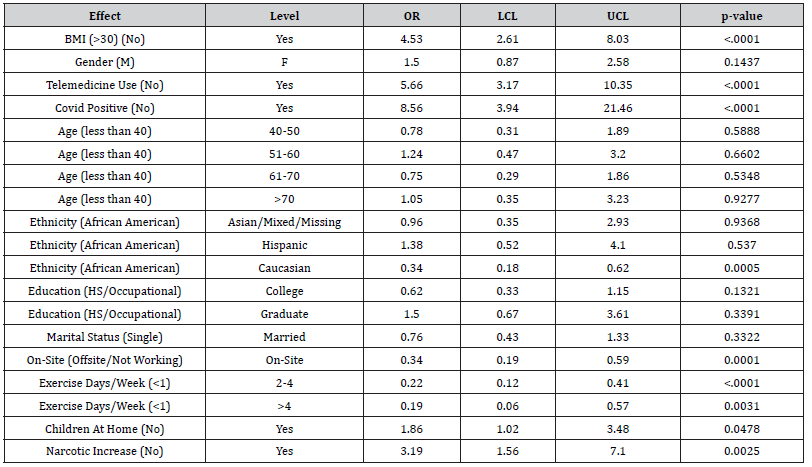
For instance, ethnicity is associated with increase in chronic pain (Table 2A), and in Table 2B, we see that people of Caucasian ethnicity have an OR of 0.34 (95% CL: 0.18 to 0.62). This indicates that Caucasians have 66% (1-0.34) lower odds of worsening chronic pain compared to African Americans (reference level). Overall, Table 2B shows that BMI (>30), narcotic use, telemedicine use, COVID-19 positive status, and having children at home were associated with increased odds of worsening of chronic pain. Furthermore, Caucasian ethnicity (relative to African American ethnicity), working on-site, exercising 2-4 times a week (relative to less than one day), and exercising more than 4 times a week (relative to less than one day), were associated with lower odds of worsening chronic pain. To understand the joint effects of these predictors, we conducted a multivariate logistic regression in which univariate effects whose p-value was <0.1 from Table 2A were included as candidate predictors of worsening of chronic pain. This resulted in a model with nine predictors, BMI (>30), ethnicity, education, working on site, exercise days per week, children at home, increase in narcotic use, use of telemedicine, and COVID-19 positive status.
The type 3 effects (effect of a given predictor when all other predictors are in the model) are shown in Table 3A below, and the odds-ratio estimates are presented in Table 3B below. The final multivariate logistic regression results from Tables 3A and 3B suggest that increase in chronic pain is associated with BMI (>30), ethnicity (marginal association), exercise frequency, narcotic use, and covid positivity. As noted earlier, the strength of the association is described by subtracting 1 from the odds ratio and multiplying it by 100; this gives the percent increase in the odds of experiencing worsening chronic pain. Specifically, Table 3B suggests that the odds of worsening chronic pain increased with those with BMI > 30 by 320% (relative to those with BMI less than 30), decreased for those of Caucasian ethnicity by 72% (relative to African American ethnicity), decreased for those exercising 2-4 times a week by 76% (relative to <1 day), marginally decreased for those exercising more than 4 days a week by 79% (relative to <1 day), and increased for those experiencing increased narcotic use by 215%, and increased for those testing positive for COVID-19 by 952%.
Table 3A:Multivariate Logistic Regression Type 3 Effects on Increase in Chronic Pain.

Table 3B:Multivariate Logistic Regression Estimates on Increase in Chronic Pain.

Discussion
The field of chronic pain faces many unique challenges in the ever-changing world many chronic pain patients found themselves in during the recent COVID-19 pandemic and the unpredictable years to come. Center for Disease Control (CDC) data shows that, between February 2020 to September 2021, there were approximately 146.6 million total infections with over 40% of the United States population was infected [2]. Thus, it is important to understand the impacts, if any, this pandemic had on worsening of chronic pain in chronic pain patients. A recent review discussed the impact of the COVID-19 on pain treatment centers specifically focused on the public health consequences of the pandemic on patients with pain, the consequences that come with lack of proper pain treatment, options of remote treatment, and clinical evidence to support remote treatment in a pandemic. The authors discuss the importance of adjusting care delivery of chronic pain patients in a pandemic and the utility of capturing provider and patient data to guide care models [3]. Although limited, recent studies have explored the impact of the pandemic on worsening of chronic pain in chronic pain patients.
A recent national survey completed in Canada in 2020 found that, despite telehealth usage during the pandemic, pain clinics reported higher pain levels, stress levels, and opioid usage among their patients. The authors discuss, in this context, that only the most urgent procedures were being performed and how patients were still waiting longer than usual for care [4]. Additionally, a cross sectional survey from 2020 of over five-hundred patients with longstanding chronic pain observed that over 70% of patients reported worsening pain and over 45% reported an increase in medication intake [5]. A recent cross-sectional study, aimed at evaluating the physical and psychosocial health impacts of the pandemic on chronic pain patients, found unchanged pain ratings but reported that pain catastrophizing scores were elevated when compared to pre-pandemic [6]. Our study specifically looked at risk factors for worsening chronic pain in chronic pain patients.
The final multivariate logistic regression results suggest that increase in chronic pain is associated with BMI (<30), ethnicity (Caucasians less likely compared to African Americans), exercise frequency (2-4 days/week less likely), increase narcotic use, and covid positivity. Telecommuting, otherwise known as “working from home”, has revolutionized the way many Americans work today. Recent research shows that, among Americans whose jobs can mainly be done from home, only 23% teleworked frequently pre-pandemic. This is in comparison to the increase seen in 2020 and 2022 where 71% and 59% of Americans whose jobs allowed for telecommuting, respectively [7]. With such a significant portion of Americans shifting to different work settings, chronic pain physicians must now consider the potential predictors associated with telecommuting and effects they may have on a patient’s quality of life, mental well-being, and ultimately chronic pain levels. A recent national poll conducted by the American Psychiatric Association found that the majority of U.S adults working from home experienced mental health impacts including isolation, loneliness, and difficulty getting away from their work [8].
A recent cross-sectional study of 1941 workers aged 20-64 with body pain prior to the study found that 15% reported worsening of their pain during their pandemic. Our study, in a univariate analysis, found that those who worked on site experienced statistically significant lower odds of increased chronic pain when compared to those that worked from home, however the statistically significant did not hold with the multivariate analysis. Indeed, more studies are needed to further explore the relationship of working from home on worsening of chronic pain in chronic pain patients. The use of narcotics in the treatment of chronic pain is a practice that requires very thorough clinical evaluation, prescription database monitoring, pain score documentation, meticulous morphine metabolic equivalent consideration, and frequent follow-up care, and random urine drug testing when indicated. This is because of the concerns for adverse effects, risk of respiratory depression, dependence, abuse potential, and opioid use disorder.
This leaves chronic pain providers with the challenge of precisely utilizing opioids, when indicated, to both provide adequate chronic pain relief but also minimize adverse associated risks. It is well understood that increases in chronic pain scores correlate with increased narcotic requirements but how does the reverse correlate? In our multivariate regression, chronic pain patients that had an increase in narcotic use had 232% higher odds of experiencing an increase in chronic pain. The dramatic increase in the utilization of telemedicine in the recent pandemic has essentially reshaped the way many chronic pain patients received their care and will continue to. A recent report from the U.S Department of Health and Human Services showed a 63-fold increase in the telehealth utilization among Medicare patients, from 840,000 telehealth visits in 2019 to 52.7 million telehealth visits in 2020 [9]. In a univariate logistic regression from our study, we found that patients who used telemedicine had statistically significant higher odds of experiencing an increase in chronic pain, however this significance did not hold true in the multivariate logistic regression analysis.
Given our findings, the role of telemedicine in the worsening of chronic pain in chronic pain patients is certainly worth discussion. It is possible that chronic pain patients who already were experiencing worsening pain sought more healthcare services and thus utilized telemedicine more often. In contrast, it could also be possible that the telemedicine services that were offered to chronic pain patients did not sufficiently address patient’s chronic pain needs and thus resulted in these patients experiencing worsening chronic pain. Undoubtedly, further studies of even larger sample sizes are warranted to further elucidate this notable positive association of the use telemedicine with worsening of chronic pain in chronic pain patients. Of important mention is the obesity epidemic in the United States and the impact of obesity on the worsening of chronic pain. According to the CDC, the obesity prevalence, based on recent data, among Americans is 41.9%. This marks an increase from 30.5% prevalence in 1999-2000. Additionally, the prevalence of severe obesity increased from 4.7% to 9.2% from 1999 to 2020.
This epidemic has resulted in a medical burden of nearly $173 billion in 2019 with obese American adults experiencing nearly $2,000 higher medical costs than those with healthy weight [10]. The association of obesity and pain is well recognized but the effect on obesity on pain scores has yet to be widely explored [11]. In our study, BMI (>30) was associated with a statistically significant 320% higher odds of experiencing worsening of chronic pain. Similarly, one cannot discuss the obesity epidemic in the United States without mention of average physical activity levels of the average American. A study conducted by the Centers for Disease Control and Prevention between 2010 and 2015 found that only 18.7% of women and 27.2% of men met federal standards for time spent exercising [12]. Our study found that chronic pain patients who exercised more certainly experienced lower odds of worsening chronic pain. Lastly, it is important to always consider the racial and ethnic disparities that exist in the treatment of chronic pain.
A recent review found that an adverse association between non-White race and the treatment of chronic pain was well supported. In this review the authors presented articles which included findings that African American patients were less likely to be prescribed opioids than Caucasian patients, less likely to fill an opioid prescription than Caucasian patients, more likely to have restricted early refills or a dose reduction within two years than Caucasian patients, and more likely to report higher levels of pain and pain-related disability than Caucasian patients [13]. In correlation with current published date, our final multivariate logistic regression suggests that the odds of worsening chronic pain decreased for those of Caucasian ethnicity by 72% (relative to African American ethnicity). Indeed, it is crucial for pain physicians to always be conscious of the ethnic disparities which exist in the field of chronic pain management and always aim toward equitable treatment of chronic pain.
Limitations
Although this is the first study of its kind to study the effect of the above-mentioned potential predictors on worsening chronic pain in chronic pain patients, it does have some limitations. These include the use of just one pain clinic for the included chronic pain population, missing patient responses in some collected surveys, and the subjective nature of pain. These anticipated limitations were taken into consideration in the planning of the study and are the reason for seeking larger sample size, a patient population that reflects the diversity of the city that the study was conducted in, and the utilization of standardized pain score assessments.
Conclusion
Univariate analysis in our study suggests BMI (>30), COVID-19 positive status, use of telemedicine, having children at home, and increase in narcotic use were associated with increased odds of worsening of chronic pain, whereas Caucasian ethnicity (relative to African American ethnicity), working on-site, exercising >1 day/week (relative to <1 day/week were associated with lower odds of worsening chronic pain. To understand the joint effects of these predictors, our multivariate analysis suggests that increase in chronic pain is associated with BMI > 30, ethnicity (Caucasians less likely compared to African Americans), exercise frequency (2-4 days/week less likely), increase narcotic use, and covid positivity. Interestingly, the association between working on-site and increase in chronic pain lose statistical significance with multivariate analysis. These findings certainly warrant further studies of even larger sample sizes to further elucidate this notable positive association.
Disclosure statement
The authors report there are no competing interests to declare. Omar Alnatour does not have any conflicts of interest. Parthasarathy Krishnamurthy does not have any conflicts of interest. Saba Javed does not have any conflict of interest.
Funding details
The authors have no financial support to report. Both authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants, patents received or pending, or royalties. No writing assistance was utilized in the production of this manuscript.
Informed consent disclosure
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved. The authors state that they have obtained verbal and written informed consent from the patient/ patients for the inclusion of their medical and treatment history within this case report.
Note: The estimates for the categorical predictors are for the comparison of the focal level (the “Level” column) relative to the reference level for the category (noted in parentheses). OR refers to odd ratio of the association. LCL (lower confidence limit) and UCL (upper confidence limit) represent 95% confidence limits in the odd ratio estimates.
Note: The estimates for the categorical predictors are for the comparison of the focal level (the “Level” column) relative to the reference level for the category (noted in parentheses). OR refers to odd ratio of the association. LCL (lower confidence limit) and UCL (upper confidence limit) represent 95% confidence limits in the odd ratio estimates.
Acknowledgement
None.
Conflict of interest
No conflict of Interest.
References
- World Health Organization (2023) WHO Coronavirus (COVID-19) Dashboard.
- Centers for Disease Control and Prevention (2021) Estimated Covid-19 Burden.
- Eccleston C, Blyth FM, Dear BF, Fisher EA, Keefe FJ, et al. (2020) Williams ACC. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 161(5): 889-893.
- Lynch ME, Williamson OD, Banfield JC (2020) COVID-19 impact and response by Canadian pain clinics: A national survey of adult pain clinics. Can J Pain 4(1): 204-209.
- Nieto R, Pardo R, Sora B, Feliu-Soler A, Luciano JV (2020) Impact of COVID-19 Lockdown Measures on Spanish People with Chronic Pain: An Online Study Survey. J Clin Med 9(11): 3558.
- Ziadni MS, You DS, Cramer EM, Anderson SR, Hettie G, et al. (2022) The impact of COVID-19 on patients with chronic pain seeking care at a tertiary pain clinic. Sci Rep 12(1): 6435.
- Parker K, Horowitz JM (2022) Covid-19 Pandemic Continues to Reshape Work in America. Pew Research Center's Social & Demographic Trends Project.
- (2021) As Americans Begin to Return to the Office, Views on Workplace Mental Health Are Mixed.
- Suran M (2022) Increased Use of Medicare Telehealth During the Pandemic. JAMA 327(4): 313.
- Centers for Disease Control and Prevention (2022) Obesity, Race/Ethnicity, and Covid-19.
- Narouze S, Souzdalnitski D (2015) Obesity and chronic pain: systematic review of prevalence and implications for pain practice. Reg Anesth Pain Med 40(2): 91-111.
- Centers for Disease Control and Prevention (2022) Adult Obesity Facts.
- Mary E Morales, R Jason Yong (2021) Racial and Ethnic Disparities in the Treatment of Chronic Pain. Pain Medicine 22(1): 75-90.
-
Omar Alnatour*, Saba Javed. The Effects Of COVID-19 On Chronic Pain Patients: An Observational Survey Study. Arch Clin Case Stud. 3(4): 2024. ACCS.MS.ID.000570.
-
Rheumatoid polyarthritis, Hypertensive, Diabetic, Anti-inflammatory drugs, Pancytopenia, Methotrexate.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






