 Case Report
Case Report
Management and Retrieval of An Accidental Postoperative Ingestion of Tongue Piercing
Keita Suto1,2*, Akira Saito1,2, Katsusuke Mori1,2, Atsushi Yoshida1,2, Hironori Yamaguchi2 and Naohiro Sata2
1Department of Surgery, Koga Red Cross Hospital, Japan
2Department of Surgery, Division of Gastroenterological, General and Transplant Surgery, Jichi Medical University, Japan
Keita Suto, Department of Surgery, Jichi Medical University Hospital, Japan
Received Date:March 19, 2024; Published Date:April 04, 2024
Abstract
Foreign body ingestion mostly occurs in children, but also occasionally in adults with mental or developmental disorders, or alcohol dependence. Although most foreign bodies pass through the gastrointestinal tract and defecate naturally, endoscopic intervention is recommended for sharp and pointed objects due to high risk of perforation. The patient was a 19-year-old woman with no underlying mental nor developmental disorders who accidentally swallowed her tongue piercing attempting to reinsert it while recovering from sedation after surgery under general anesthesia. We carefully monitored her with daily abdominal X-rays from the first postoperative day expecting it to pass with natural defecation. However, it remained lodged in the ileocecal region from the second to third postoperative day and was safely retrieved with colonoscopy. Her subsequent course was uneventful without any complications. In Japan, tongue piercings are still not popular, and risks are still largely unknown. In case of accidental ingestion, careful monitoring with abdominal X-rays is important for timely endoscopic or surgical intervention.
Keywords: Foreign body; ingestion; tongue piercing
Abbreviations: BMI: Body mass index
Introduction
Most foreign body ingestions occur in children and rarely in adults [1,2]. In adults, it is more common in people with mental illness or developmental disabilities, alcoholics, and edentulous people [3-5]. More than 80% of foreign bodies are likely to pass without the need for intervention [6,7], but the rate of endoscopic intervention can be much higher for intentional ingestion. Ingestion of sharp, pointed objects, such as animal or fish bones, bread bag clips, magnets, or medication blister packs increases the risk of perforation [8-13]. Here, we present a rare case in which a 19-year-old woman with no underlying medical conditions such as mental illness or developmental disability accidentally ingested her tongue piercing postoperatively while recovering from surgery under general anesthesia. The work reported here is in line with the SCARE standards [14].
Case Presentation
The patient is a 19-year-old female (height 157.1cm, weight
49.1kg, BMI 19.89) with no particular medical history. She took no
regular medications and had no allergies. One month earlier she
had been diagnosed with acute appendicitis at our hospital which
improved with conservative treatment and was discharged. She was
re-admitted for a planned interval appendectomy. Laparoscopic
appendectomy was carried out under general anesthesia. The
surgery was uneventful. Furthermore, no abnormalities were
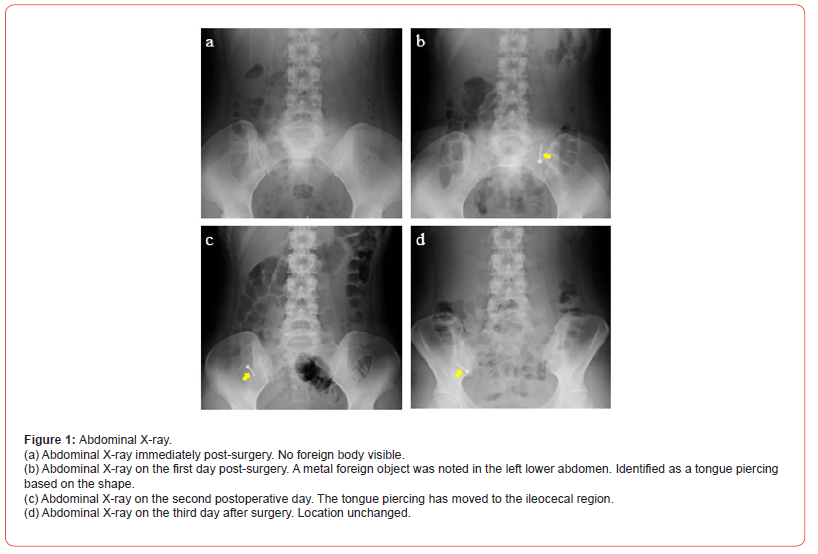
identified on postoperative abdominal X-ray examination (Figure
1a). After awakening from general anesthesia, she returned to
her room. An X-ray of her abdomen on the first postoperative day
revealed a metallic component in her abdomen (Figure 1b). Since
the piercing was not visible in the abdominal X-ray immediately
after surgery, it was concluded that she had accidentally ingested it
while wearing it at night after she had re-inserted it post-surgery.
There were no abdominal symptoms, and there were no abnormal
findings in the blood findings as shown below:
a) White blood cells count 8,160 cells/μl (3300–8800).
b) Hemoglobin 12.1 g/dl (11.0–16.0).
c) Hematocrit 36.1 % (30.5–50.3).
d) Platelet count 18.7 × 104/μl (12–28).
e) C-reactive protein 0.82 mg/dl (0–0.3).
f) Aspartate aminotransferase 13 IU/L (10–33).
g) Alanine aminotransferase 8 IU/ L (5–33).
h) Lactate dehydrogenase 132 IU/L (89–231).
i) Total bilirubin 1.2 mg/dL (0.2–1.2).
j) Blood urea nitrogen 6.7 mg/dL (8–20).
k) Creatinine 0.53 mg/dL (0.5–1.11).
l) Sodium 139.4 mEq/L (136–147).
m) Potassium 4.2 mEq/L (3.6–5.0).
n) Chlorine 103.7 mEq/L (98–109).
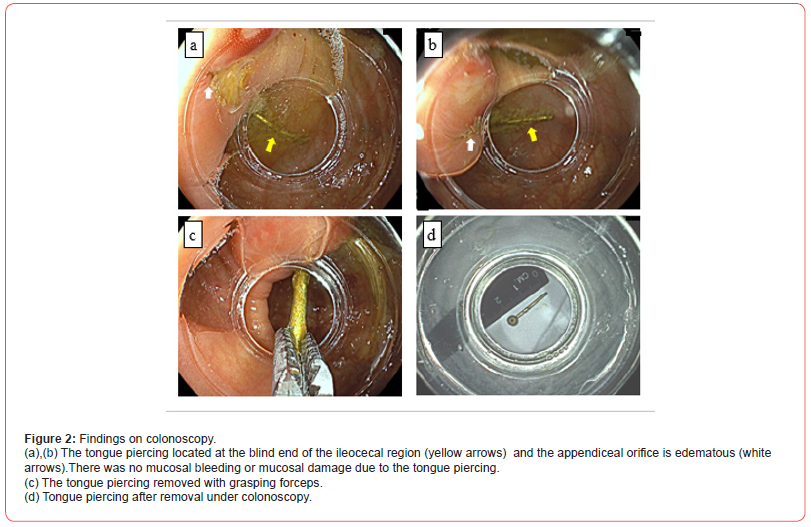
Abdominal X-ray examination showed no free air, and the tongue piercing was considered located in the small intestine. We decided to follow up with daily abdominal X-rays expecting the piercing would be excreted by natural defecation. Observation on the second postoperative day suggested it had moved to the ileocecal region or the ascending colon (Figure 1c). Abdominal X-ray on the third postoperative day showed no change in position (Figure 1d), so we decided on retrieval through colonoscopy. Colonoscopy results showed no mucosal bleeding or mucosal damage due to the tongue piercing, and it was confirmed located at the blind end of the ileocecal region. (Figures 2a&2b). The appendiceal orifice had become edematous due to postoperative effects, and the tongue piercing was retrieved using grasping forceps of colonoscopy (Figure 2c). It was made of surgical stainless steel with a total length of 2.5 cm and a thickness of 14G (Figure 2d). The patient resumed eating on the same evening. Abdominal symptoms remained unremarkable, so she was discharged on the fourth postoperative day. Thereafter, the patient progressed uneventfully without any complications after visiting the outpatient clinic.
Discussion
Many cases of foreign body ingestion are reported each year, and 80% of these cases occur in children, typically between 6 months and 3 years of age [15]. Foreign body ingestion in adults is rare compared to children [16] and may occur for iatrogenic or individual satisfaction reasons [17]. It is observed in people with alcoholism, mental disorders, or developmental disabilities, as well as for secondary purposes such as incarcerated individuals attempting release from prison [3]. Most objects are foods such as meat and fish bones, but dentures, nails, and screws [18] may also be ingested. Ingested foreign objects pass the gastrointestinal tract in 80% of cases, endoscopy is required in 20%, and <1% requires surgical procedure [16]. Intentional ingestion of sharp metal objects is more prone to complications. Although the majority pass without incident, up to 30–35% may penetrate the wall of the gastrointestinal tract and endoscopically retrieval is recommended [19-22]. Otherwise, they may be followed with daily radiographs to document their passage, and surgical intervention should be considered for objects that fail to progress after 3 days [23,24].
In this case, the patient had no history of mental illness, disability, nor incarceration, and accidentally swallowed an approximately 3cm-long tongue piercing likely from incorrect insertion while recovering from sedation. The catch on one side had come off, and the tip of the 14G straight barbell was exposed and sharp. There was a perceived risk of intestinal perforation due to the sharp metal, but since it was in the small intestine, fasting was prescribed with daily abdominal X-rays to confirm its position. After two days, the tongue piercing was confirmed to have reached the large intestine and was retrieved with colonoscopy. As a result, the patient progressed without complications. A past case has been reported of an accidentally swallowed tongue piercing entering the appendix lumen and causing appendicitis [25]. It has been theorized that the metallic foreign objects heavier than intestinal contents Üauses it to be stayed in the cecum, and its lower anatomical position causes the object to move toward the appendix [26].
Since the case here was post-appendectomy, the tongue piercing did not enter the appendiceal cavity. However, endoscopic findings confirmed its location at the blind end of the ileocecal region near the appendiceal orifice. Therefore, if not retrieved endoscopically, it would not have been excreted through natural defecation and could have potentially caused complications. This case is the first case report in which an accidentally swallowed tongue piercing was removed by colonoscopy, careful monitoring with abdominal X-rays and timely endoscopic or surgical intervention are essential. In addition, young people are increasingly interested in body art [27]. However, in Japan there is still insufficient awareness among users and medical professionals of how to manage tongue piercings and their associated complications. Awareness of their risks during peri- and post-operative management is necessary.
Acknowledgment
We thank all staff of the Koga Red Cross Hospital who contributed to this report.
Conflict of interest
No conflict of interest.
References
- Cheng W, Tam PK (1999) Foreign-body ingestion in children: experience with 1265 cases. J Pediatr Surg 34(10): 1472-1476.
- Hachimi-Idrissi S, Come L, Vandenpias Y (1998) Management of ingested foreign bodies in childhood: our experience and review of the literature. Eur J Emerg Med 5(3): 319-323.
- Blaho KE, Merigian KS, Winbery SL, Cockrell M (1998) Foreign body ingestions in the emergency department: case reports and review of treatment. J Emerg Med 16(1): 21-26.
- Kamal Ihab, Thompson John, Paquette M Dana (1999) The hazards of vinyl glove ingestion in the mentally retarded patient with pica: new implications for surgical management. Can J Surg 42(3): 201-204.
- Abdullah BJ, Teong LK, Mahadevan J, Jalaudin A (1998) Dental prosthesis ingested and impacted in the esophagus and orolaryngopharynx. J Otolaryngol 27(4): 190-194.
- Carp L (1927) Foreign bodies in the intestine. Ann Surg 85(4): 575-591.
- Pellerin D, Fortier-Beaulieu M, Gueguen J (1969) The fate of swallowed foreign bodies experience of 1250 instances of sub-diaphragmatic foreign bodies in children. Progr Pediatr Radiol 2: 286-302.
- Selivanov V, Sheldon CF, Cello JP, Crass RA (1984) Management of foreign body ingestion. Ann Surg 199(2): 187-191.
- Newell KJ, Taylor B, Walton JC, Tweedie EJ (2000) Plastic bread- bag clips in the gastrointestinal tract: report of 5 cases and review of the literature. CMAJ 162(4): 527-529.
- Yamada T, Sato H, Seki M, Kitagawa S, Nakagawa M (1996) Successful salvage of aortoesophageal fistula caused by a fish bone. Ann Thorac Surg 61(6): 1843-1845.
- Yamaguchi H, Yamashita H, Yamauchi H, Suzuki T, Ishimaru M (2005) Intestinal perforation caused by stagnated press-through packages. Surgery 137(6): 661-662.
- Palta Renee, Sahota Amandeep, Bemarki Ali, Salama Paul, Simpson Nicole (2009) Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc 69(3): 426-433.
- Weiland T Steven, Schurr J Michael (2002) Conservative management of ingested foreign bodies. J Gastrointest Surg 6(3): 496-500.
- Riaz A Agha, Thomas Franchi, Catrin Sohrabi, Ginimol Mathew (2020) The SCARE2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 84: 226-230.
- Robert Wyllie (2006) Foreign bodies in the gastrointestinal tract. Curr Opin Pediatr 18(5): 563-564.
- WT Wu, Ct Chiu, CJ Kuo, CJ Lin, YY Chu (2011) Endoscopic management of suspected esophageal foreignbody in adults. Dis Esophagus 24(3): 131-137.
- Jun Hyung Lee, Hyun Cheol Kim, Dal Mo Yang, Sang Won Kim, Wook Jin (2012) What is the role of plain radiography in patients with foreign bodies in the gastrointestinal tract? Clin Imaging 36(3): 447-454.
- Ambe Peter, Sebastian A Weber, Mathias Schauer, Wolfram T Knoefel (2012) Swallowed foreign bodies in adults. Dtsch Arztebl Int 109(50): 869-875.
- Jia-Jang Chang, Cho-Li Yen (2004) Endoscopic retrieval of multiple fragmented gastric bamboo chopsticks by using a flexible overtube. World J Gastroenterol 10(5): 769-770.
- Carp L (1927) Foreign bodies in the intestine. Ann Surg 85(4): 575-591.
- Vizcarrondo FJ, Brady PG, Nord HJ (1983) Foreign bodies of the upper gastrointestinal tract. Gastrointest Endosc 29(3): 208-210.
- Rosch W, Classen M (1972) Fiberendoscopic foreign body removal from the upper gastrointestinal tract. Endoscopy 4(4): 193-197.
- Webb WA (1995) Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc 41(1): 39-51.
- Milton T Smith, Roy K H Wong (2007) Foreign bodies. Gastrointest Endosc Clin N Am 17(2): 361-382.
- Rossana Cheng He, Tamar Nobel, Alexander J. Greenstein (2021) A case report of foreign body appendicitis caused by tongue piercing ingestion. Int J Surg Case Rep 81: 105808.
- Zdravko Perko, Kanito Bilan, Zenon Pogorelic, Nikica Druzijanic, Darko Srsen (2008) Acute appendicitis and ileal perforation with a toothpicktreated by laparoscopy. Coll Antropol 32(1): 307-309.
- Francesco Covello, Camilla Salerno, Valentina Giovannini, Denise Corridore, Livia Ottolenghi (2020) Piercing and Oral Health: A Study on the Knowledge of Risks and Complications. Int J Environ Res Public Health 17(2): 613.
-
Keita Suto*, Akira Saito, Katsusuke Mori, Atsushi Yoshida, Hironori Yamaguchi and Naohiro Sata. Management and Retrieval of An Accidental Postoperative Ingestion of Tongue Piercing. Arch Clin Case Stud. 3(5): 2024. ACCS.MS.ID.000574.
-
Foreign body; ingestion; tongue piercing; iris publishers; iris publisher’s group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






