 Review Article
Review Article
The Role of Genetic Mutations in Genes TSC1 & TSC2 in Bourneville Syndrome
Shahin Asadi*, Soheil Nemati Arzeloo and Mahsa Jamali
Director of the Division of Medical Genetics and Molecular Research, Medical Genetics, Tabriz, Iran
Shahin Asadi, Director of the Division of Medical Genetics and Molecular Research, Tabriz, Iran.
Received Date:August 05, 2019; Published Date:August 22, 2019
Abstract
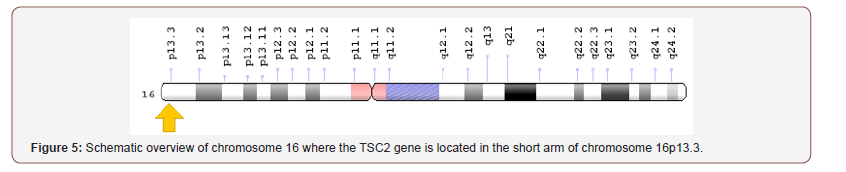
Bourneville Syndrome, also known as Tuberous Sclerosis Complex Disorder, is a genetic disorder characterized by the growth of numerous non-cancerous tumors in many parts of the body. Bourneville Syndrome often affects the brain, which causes seizures, behavioral problems such as hyperactivity and aggression, and mental disorders or learning problems. Bourneville syndrome is caused by a mutation of the TSC1 gene located on the long arm of chromosome 9 at 9q34.13 or the TSC2 gene at the short arm of chromosome 16 at 16p13.3.
Keywords: Bourneville syndrome; Tuberous sclerosis complex disorder; TSC1 & TSC2 genes; Genetics Disorder
Overview of Bourneville Syndrome
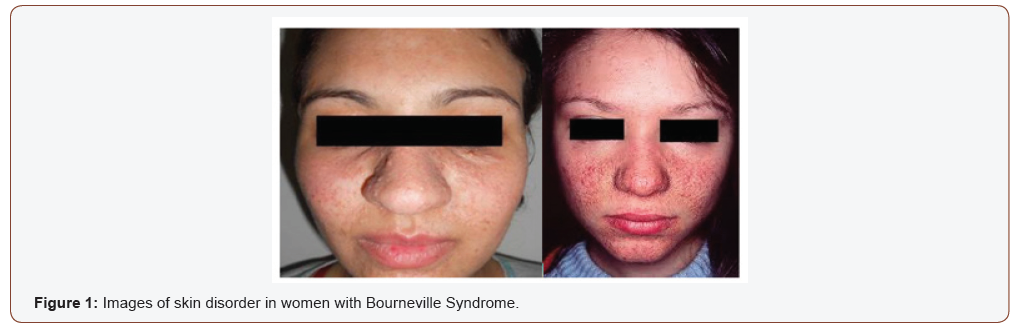
Bourneville Syndrome, also known as Tuberous Sclerosis Complex Disorder, is a genetic disorder characterized by the growth of numerous non-cancerous tumors in many parts of the body. These tumors can develop in the skin, brain, kidneys and other organs, and in some cases can cause significant health problems. Bourneville Syndrome also causes developmental problems and the signs and symptoms of the disease vary from person to person [1] (Figure 1).
Clinical Signs and Symptoms of Bourneville Syndrome
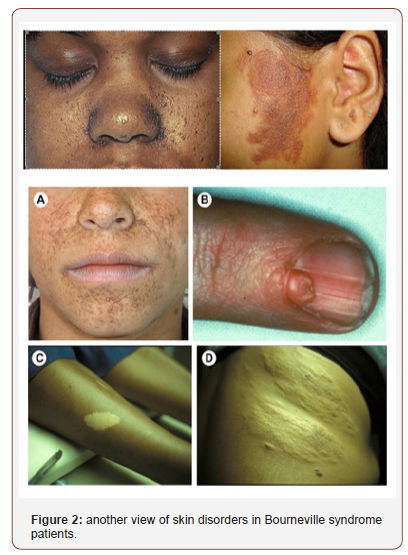
Almost everyone with this syndrome has skin disorders, including patches of unusually colored and thick skin, which grow beneath the nails. Facial tumors, called angiofibromas, also begin in childhood [2]. Bourneville syndrome often affects the brain, which causes seizures, behavioral problems such as hyperactivity and aggression, and mental disorders or learning problems. Some children with this syndrome have the characteristic features of autism, which is a developmental disorder that affects communication and social interactions. Benign brain tumors can also occur in people with Bourneville syndrome. These tumors can cause serious or life-threatening complications [3] (Figure 2).
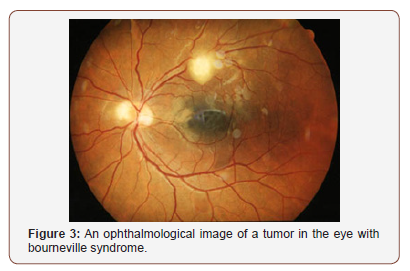
Kidney tumors are common in people with bourneville syndrome. This growth of kidney tumors can cause severe problems with kidney function and in some cases can be life threatening. In addition, tumors also grow on the heart, lungs, and light-sensitive tissue behind the eye (retina) [3] (Figure 3).
Etiology of Bourneville Syndrome
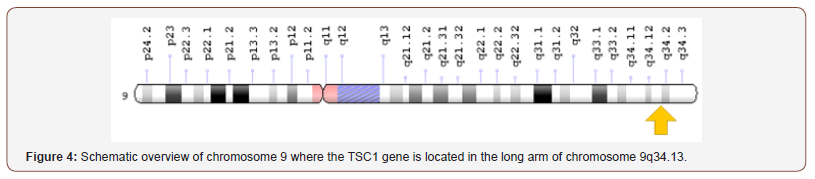
Bourneville syndrome is caused by a mutation of the TSC1 gene located on the long arm of chromosome 9 at 9q34.13 or the TSC2 gene at the short arm of chromosome 16 at 16p13.3. The TSC1 and TSC2 genes, respectively, provide instructions for the synthesis of hamartin and tubulin proteins, respectively. Inside the cells, these two proteins are likely to work together to help regulate cell growth and cell size. These proteins actually act as tumor suppressors that typically prevent cells from growing or dividing too fast or uncontrollably [4].
People with bourneville syndrome are born with a mutated copy of the TSC1 or TSC2 gene in each cell. This mutation prevents the synthesis of the hamartin or tubulin protein from altered copy of these genes. However, normally enough protein from the normal copy of the gene is produced efficiently to regulate cell growth. For some types of tumors that need to grow, a second mutation involving another copy of the TSC1 or TSC2 gene must occur in certain cells throughout one’s lifetime [5] (Figure 4)
When both copies of the TSC1 gene mutate in a particular cell, the cell cannot produce functional hamartin protein. Cells with duplicated copies of the TSC2 gene are unable to produce any functional tobin proteins. The loss of these proteins allows the cell to continue to grow and divide in an uncontrolled manner for tumor formation. In people with bourneville syndrome, mutations in the TSC1 or TSC2 gene variant usually occur in several cells and throughout the life of the patient. Loss of hamartin or tobin in different types of cells results in the growth of tumors in many different organs and tissues [6] (Figure 5).
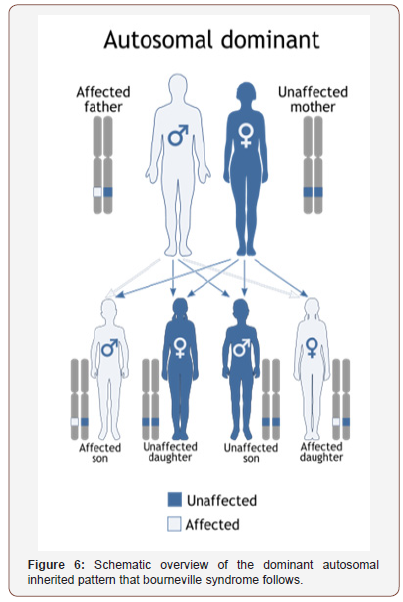
Bourneville syndrome follows the dominant autosomal inherited pattern. Therefore, a version of the mutated TSC1 or TSC2 gene (whether parent or parent) is required for this syndrome and the chance of having a child with this syndrome in the autosomal dominant state is 50% for each possible pregnancy [7] (Figure 6).
Frequency of Bourneville Syndrome
Bourneville syndrome is a genetic disorder with a prevalence of about 1 in 6,000. Tuberous sclerosis is a rare genetic disorder that affects 1 in 6,000 newborns in the United States. Approximately 40,000 to 80,000 people in the United States have tuberous sclerosis. The prevalence in Europe is estimated to be approximately 1 in 25,000 to 1 in 11,300. As many as 2 million people worldwide are believed to have the disorder. Males and females are affected in equal numbers and the disorder occurs in all races and ethnic groups [8].
Diagnosis of Bourneville Syndrome
Bourneville syndrome is diagnosed based on clinical and clinical findings of patients and some pathological, oncological, and neurological tests. The most accurate method to detect this syndrome is molecular genetic testing for the TSC1 or TSC2 gene to determine the presence of possible mutations. Diagnosis is based on presence of major (cortical dysplasias; subependymal nodules; SEGA; hypomelanotic macules (≥3, diameter ≥5 mm); shagreen patch; angiofibromas (≥3) or fibrous cephalic plaque; multiple retinal hamartomas; ungual fibromas (≥2); CR; LAM; AML (≥2)) and minor (dental enamel pits (≥3); intraoral fibromas; confetti skin lesions; nonrenal hamartoma; multiple renal cysts; retinal achromatic patches) features. A definite diagnosis is defined as presence of ≥2 major features or 1 major and ≥2 minor features. Possible TSC is considered in the presence of 1 major or ≥2 minor features. TSC can be diagnosed by genetic screening regardless of the clinical findings [9].
The Therapeutic Pathways of Bourneville Syndrome
The treatment and management strategy for bourneville syndrome is symptomatic and supportive. The treatment may be coordinated by a team of specialists including nephrologists, neurologists, oncologists, surgeons and other health care professionals. There is no effective treatment for this syndrome and all clinical measures are to alleviate the suffering of the patients. Genetic counseling is also needed for all parents who want a healthy child. Treatment may require the coordinated efforts of a team of specialists. Pediatricians and general internists, neurologists, dermatologists, cardiologists, dental specialists, eye specialists, psychiatrists, and other healthcare professionals may need to systematically and comprehensively plan an affect child’s treatment. Genetic counseling will be of benefit for affected individuals and their families [10].
The treatment for tuberous sclerosis is supportive and symptomatic. Early developmental intervention is important to ensure that affected children reach their potential. Most affected children will benefit from occupational, physical and speech therapy. Various methods of rehabilitative and behavioral therapy may be beneficial. It is essential that therapies are continued on a year-round basis to promote development of new skills and to prevent regression. Additional medical, social and/or vocational services including special remedial education may be necessary. Psychosocial support for the entire family is essential as well [10].
Anti-seizure drugs (anticonvulsants) may be prescribed to control seizures. The specific drug that is used will depend on several factors including the specific type of seizure, an affected individual’s age, other organ systems that are affected, and the severity of symptoms. Conventional anticonvulsants drugs that may be administered include phenobarbital, phenytoin (Dilantin), clonazepam (Clonopin), valproic acid (Depakene), carbamazepine (Tegretol), ethosuximide (Zarontin), or acetazolemide (Diamox). All these anticonvulsants have potential side effects and require careful monitoring by a physician [10].
Discussion and Conclusion
Bourneville Syndrome often affects the brain, which causes seizures, behavioral problems such as hyperactivity and aggression, and mental disorders or learning problems. Bourneville syndrome is caused by a mutation of the TSC1 gene located on the long arm of chromosome 9 at 9q34.13 or the TSC2 gene at the short arm of chromosome 16 at 16p13.3. Vigabatrin (Sabril) was approved in 2009 by FDA to treat infantile spasms in children ages 1 month to 2 years. Treatment of children with tuberous sclerosis and infantile spasms with vigabatrin has been found to be effective. Visual field loss is an important safety concern with the use of this medication. The FDA has also approved adreno-corticotrophic hormone or ACTH (Acthar gel) for the treatment of infantile spasms. This medication has also been used to treat infants with tuberous sclerosis. These medications are used cautiously because of their side effects [1-3].
No specific anti-seizure medication works for all affected individuals. Often, a combination of different drugs may be required to treat some individuals. Sometimes, seizures can be difficult to treat and medications that initially worked will no longer provide benefit (refractory seizures). In some instances, surgery may be necessary to help to control seizures that don’t respond or stop responding to medications [4-5]. Surgery may be necessary if the ability of a particular organ to function properly is impaired by the presence of a tumor. For example, the obstruction of cerebrospinal fluid (CSF) circulation inside the brain (intracranial hypertension) because of a benign tumor may require a shunting procedure to drain the liquid or the surgical removal of the tumor [6-7].
In 2012, the U.S. Food and Drug Administration (FDA) approved the use of everolimus (Afinitor) for the treatment of children and adults with tuberous sclerosis who have a subependymal giant cell astrocytoma that cannot be removed or can be only partially removed by surgery [8-9]. The FDA also approved everolimus for the treatment of adults with tuberous sclerosis who have an angiomyolipoma of the kidneys that does not require surgery right away. In some instances, angiomyolipomas will require surgery. Large cystic lesions of the kidneys may also require surgical decompression or removal. Cutting off the blood supply (arterial embolization) to a kidney tumor may be used to shrink down the size of the tumor. Embolization is usually followed by treatment with corticosteroids and surgical removal (resection) of the tumor that spares the kidney or by destruction (ablation) of the tumor [10].
A benign tumor inside the heart (rhabdomyoma) may not cause symptoms and may not require treatment as they often regress on their won. If symptomatic, however, surgical removal (resection) may be necessary. Reports in the medical literature have detailed the off-label use of mTOR inhibitors to treat these tumors with positive results. Some affected individuals may be prescribed certain medications to treat irregular heartbeats (arrhythmias) [10]. Individuals taking mTOR inhibitors for internal tumors (e.g. SEGAs or angiomyolipomas) may see improvement in skin lesions. Topical formulations of mTOR inhibitors have shown promise in treating facial angiofibromas. Individuals with no immediate indication for mTOR inhibitor treatment, may undergo certain procedures to improve the appearance of skin lesions including dermabrasion, laser therapy, or surgical removal (excision) of a lesion [10].
In May of 2015, the FDA approved the use of mTOR inhibitors for the treatment of lung complications such as LAM in individuals with tuberous sclerosis. Because LAM occurs most often in young women of childbearing age, researchers have speculated that female hormones such as estrogen play a role in the development of the disorder. A link between LAM and female hormones has not been proven. However, many physicians have explored the use of agents that lower the production or effects of estrogen in the body. The results have varied greatly among individuals. Such agents may include medroxyprogesterone acetate. Estrogen-containing medications and dietary supplements should be discontinued in patients with LAM [10].
Supplemental oxygen therapy may be necessary for some individuals with impaired lung function. In individuals with severe lung disease that is resistant to treatment, a lung transplant may ultimately become necessary [10].
Acknowledgement
None.
Conflicts of Interest
No Conflicts of Interest.
References
- Crino PB, Nathanson KL, Henske EP (2006) The tuberous sclerosis complex. N Engl J Med 355(13): 1345-1356.
- Curatolo P, Bombardieri R, Jozwiak S (2008) Tuberous sclerosis. Lancet 372(9639): 657-668.
- Franz DN, Bissler JJ, Mc Cormack FX (2010) Tuberous sclerosis complex: neurological, renal and pulmonary manifestations. Neuropediatrics 41(5): 199-208.
- Hyman MH, Whittemore VH (2000) National Institutes of Health consensus conference: tuberous sclerosis complex. Arch Neurol 57(5): 662-665.
- Lewis JC, Thomas HV, Murphy KC, Sampson JR (2004) Genotype and psychological phenotype in tuberous sclerosis. J Med Genet. 41(3):203-207.
- Maria BL, Deidrick KM, Roach ES, Gutmann DH (2004) Tuberous sclerosis complex: pathogenesis, diagnosis, strategies, therapies, and future research directions. J Child Neurol 19(9): 632-642.
- Northrup H, Koenig MK, Pearson DA, Au KS (1999) Tuberous Sclerosis Complex. In: Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A (eds.) GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle, Washington 1993-2017.
- Orlova KA, Crino PB (2010) The tuberous sclerosis complex. Ann N Y Acad Sci 1184: 87-105.
- Rosser T, Panigrahy A, Mc Clintock W (2006) The diverse clinical manifestations of tuberous sclerosis complex: a review. Semin Pediatr Neurol 13(1): 27-36.
- Schwartz RA, Fernández G, Kotulska K, Jóźwiak S (2007) Tuberous sclerosis complex: advances in diagnosis, genetics, and management. J Am Acad Dermatol 57(2): 189-202.
-
Shahin Asadi, Soheil Nemati Arzeloo, Mahsa Jamali. The Role of Genetic Mutations in Genes TSC1 & TSC2 in Bourneville Syndrome. Arch Biomed Eng & Biotechnol. 2(4): 2019. ABEB.MS.ID.000541.
-
Bourneville syndrome, Tuberous sclerosis complex disorder, TSC1 & TSC2 genes, Genetics Disorder, Bourneville syndrome, Skin, Brain, Kidneys, Tuberous sclerosis, Facial tumors, Angiofibromas
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
- Abstract
- Overview of Bourneville Syndrome
- Clinical Signs and Symptoms of Bourneville Syndrome
- Etiology of Bourneville Syndrome
- Frequency of Bourneville Syndrome
- Diagnosis of Bourneville Syndrome
- The Therapeutic Pathways of Bourneville Syndrome
- Discussion and Conclusion
- Acknowledgement
- Conflicts of Interest
- References






