 Research Article
Research Article
Pinch Endurance in Elderly People
So Miyahara1*, Yoshihiro Tanikawa1, Hideo Hirai1, Akira Otsuka2 and Seiji Togashi1
1Department of Rehabilitation, Faculty of Health Sciences, Hiroshima Cosmopolitan University, Hiroshima, Japan
2Department of Physical Therapy, Faculty of Health and Welfare, Prefectural University of Hiroshima, Mihara City, Hiroshima, Japan
So Miyahara, Department of Rehabilitation, Faculty of Health Sciences, Hiroshima Cosmopolitan University, 3-2-1 Otsukahigashi, Asaminami ward, Hiroshima, 731-3166, Japan.
Received Date: September 16, 2021; Published Date: September 28, 2021
Abstract
There are many items to measure physical functions, and assessment using a hand, such as handgrip strength, draws a great deal of interest. Pinch strength, as well as handgrip strength, can be measured in a short period of time, which makes it a common measurement method used in a clinical setting. However, there are no reports that have evaluated its endurance. Sixteen subjects (78.5±3.2 years old) living in Hiroshima city were measured their dominant hand pinch strength with maximum force for 20 seconds. The average value per second was calculated from the results. Fifteen students (21.5±0.6 years old, hereinafter referred to as the “younger group”) were also measured in the same way for comparison.
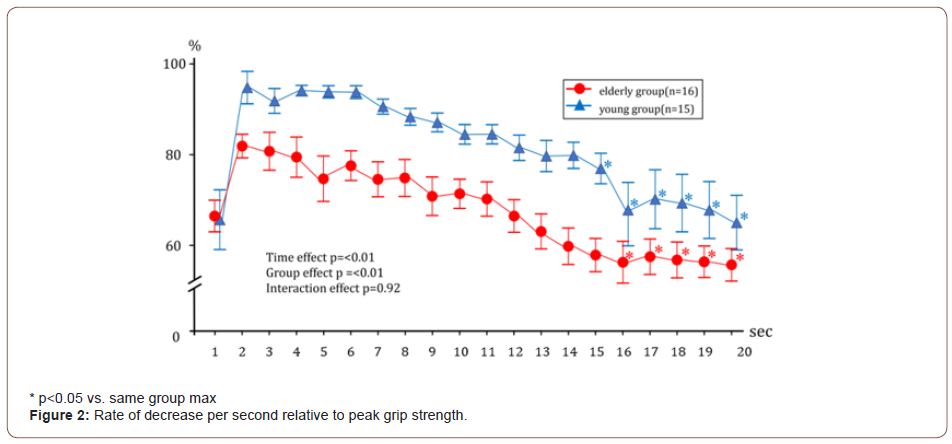
Result: The maximum pinch strength in 20 seconds was lower in the elderly group than that in the younger group (4.1±1.3 N vs. 6.8±1.2 N, p<0.01). Both groups showed maximum strength when two seconds had passed. The elderly group showed no significant decrease in pinch strength over 20 seconds, while the younger group showed decrease only after 20 seconds had passed, however, there was no difference between the groups (Group*Time effect p=0.82). In terms of decrease rate from the maximum value, elderly and younger group showed a significant decrease, however there was no difference between the groups (after 16 seconds vs. 15 seconds, Group*Time effect p=0.92).
Conclusion: Measurement of pinch endurance showed no difference in transition of strength in both the elderly and the younger groups: a certain level of strength from the maximum value was able to be exerted. The results could be useful as a reference for demonstrating enduring strength in daily life and sports. We would like to continue to study its effect on circulatory hemodynamics, the comparison with other pinch strength, and the relationship with finger coordination.
Keywords:Pinch Endurance; Elderly
Abbreviations:PD: Pinch Endurance
Introduction
In many countries, there are lots of measurable items of physical function for their citizens. In recent years, there has been a great deal of clinical and research interest in sarcopenia and frailty as a means of evaluating prediction of the event [1-4]. As for evaluation of sarcopenia and frailty, many theories have been proposed to relate them to various evaluation methods [5,6]. Asian Working Group for Sarcopenia (AWGS) has also focused on handgrip strength and has identified lifestyle interventions [7], particularly exercise and nutrition, as the mainstay of treatment and prevention to improve low muscle strength [8,9].
Like handgrip strength, pinch strength is an index for evaluating a hand [10]. Previous reports suggest that both handgrip strength and pinch strength can be used as clinical criteria [11]. We previously studied and reported on handgrip endurance in older and younger adults [12]. However, pinch endurance has not been reported. Therefore, in order to find out the possibility that pinch endurance can be used as an evaluation index, we measured pinch endurance in elderly and younger people and the change over time under the hypothesis that the results would be similar to those of handgrip endurance.
Materials and Methods
The subjects were 16 elderly people (AHA/ACC classification Stage A/B [13], 2 males and 14 females, 78.5±3.2 years old) aged 65 or older living in Hiroshima city, who do exercise of light intensity (<2 METs) once a week, and 15 healthy young people (9 males and 6 females, 21.5±0.6 years old) as a comparison group. Measurements were conducted in April 2021 for the elderly group and in September 2021 for the younger group, while taking care to prevent the spread of infection by COVID-19. Subjects suffering from diseases that may affect pinch strength measurement were not measured (those with severe heart failure, end-stage renal failure, malignant tumors, dementia, severe chronic lung diseases, and those unable to walk more than 20 m). The study was approved by the Hiroshima cosmopolitan university internal ethics committee, and the data were anonymized based on privacy protection.
In order to measure pinch strength and endurance, participants were asked to sit on a chair without leaning back, with both knees bent at a right angle, both soles touching on the ground, elbows bent at a right angle, and forearms and wrists in a neutral limb position [14]. Participants used their dominant hand to measure for 20 seconds with maximum strength. Bellies of the thumb and the index finger were used for pinching. The pinch strength measurement device used was an attachment for pinch strength (T.K.K. 1269m, Takei Scientific Instruments Co., Ltd.). The measurement unit for the maximum pinch strength is newton (N). A strain amplifier (T.K.K.1268 Takei Scientific Instruments Co., Ltd.) and an A/D converter (T.K.K.5721 Takei Scientific Instruments Co., Ltd.) were used to digitally output (v) the measurement results. The results of participants’ pinch endurance were calculated by converting the value obtained in 1/100 seconds into the average per second. Analysis was performed using commercial software (SPSS ver.26, IBM). In the data, the values are expressed as average ± SE in the figures. Continuous variables were presented as mean values, and a p-value of less than 0.05 was considered statistically significant.
Result and Discussion
Result
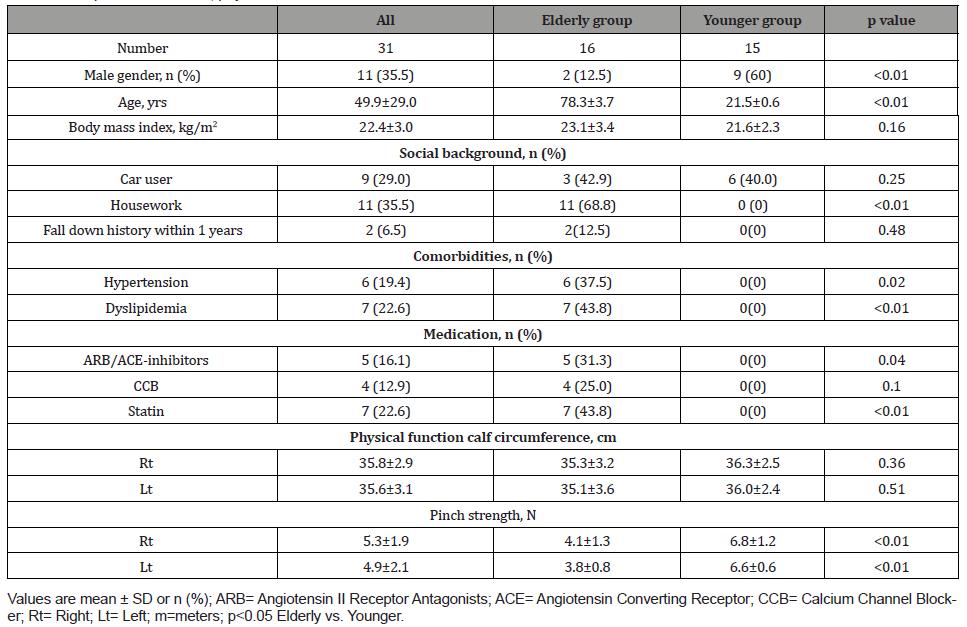
Social background showed a difference in age between the elderly and the younger groups (<0.01). Twenty-second maximum pinch strength showed difference (4.1±1.3N vs. 6.8±1.2N, p<0.01). Pinch endurance for 20 seconds showed no difference between the elderly and the younger groups (Group*Time effect p=0.82). Average pinch strength per second reached its maximum value when two seconds had passed both in the elderly and the younger group. The younger group showed a significant decrease in the maximum value when 20 seconds had passed, while the elderly group showed no decrease in the maximum value. The decline rate per second relative to the maximum value showed no difference between the elderly and young groups (Group*Time effect p=0.92). As for the decline rate to the maximum value when two seconds had passed, the elderly group showed a significant decrease after 16 seconds, while the younger group showed a significant decrease after 15 seconds had passed (Figure 1,2) (Table 1).
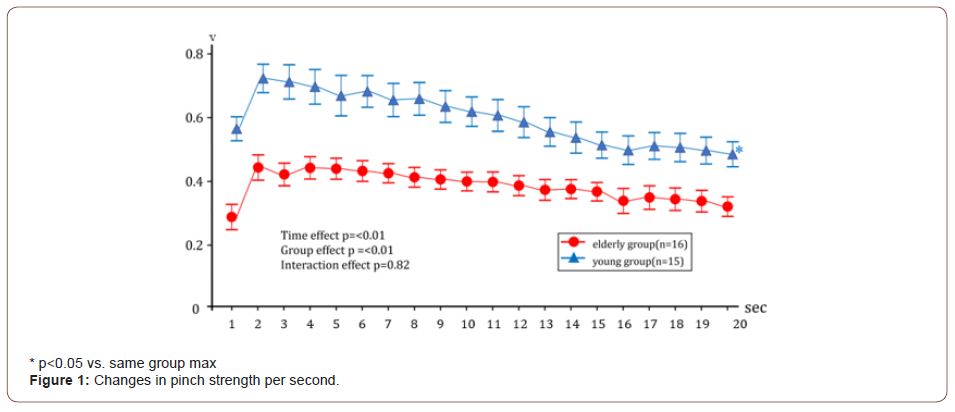
Table 1: People characteristics, physical function data.
Discussion
We measured pinch endurance of the dominant hand with maximum strength for 20 seconds in the elderly group and examined differences between the elderly and the younger group, the change rate over time (seconds), and the measurement time.
Pinch endurance and strength within elderly people
It has been reported that there is no correlation between pinch strength and handgrip strength in men with type 2 diabetes [15]. It has also been reported that handgrip endurance was different between the elderly and younger groups (interaction effect p<0.01) [12]. Handgrip endurance has been reported to show a significant decrease after 16 seconds compared to the maximum value in the younger group, while the elderly group showed no decrease after 20 seconds. In the study of pinch endurance here, the elderly group showed no decrease compared to the maximum value after 20 seconds, while the younger group showed decrease only after 20 seconds had passed. However, there was no difference in the passage of time between the two groups (Group*Time effect p=0.92), and pinch endurance did not show the same result as handgrip endurance.
In a study of students up to 16 years old, pinch strength has been reported to correlate with BMI [14]. In our study, the elderly and the young groups showed a difference in maximum pinch strength (p<0.01), but not in BMI (p=0.16). It has also been reported that pinch strength correlates with physical activity level in young people, and that pinch strength correlates with hand strength depending on lifestyle (e.g., work engagement) in elderly people over 60 years old (16). The group of elderly people measured in this study were not engaged in any work in their residential area. Another study has reported that engaging in household activities promotes the maintenance of physical activity. Among the participants, we calculated pinch strength between the groups with and without housework engagement and found no difference (4.1±1.1N vs. 4.1±1.7N, p=0.91).
Pinch strength measurement time
Pinch strength has been measured in a variety of ways from 3 to 10 seconds [16,17]. Handgrip strength has been measured in 3 to 5 seconds, and it has been reported that the maximum value can be measured within 5 seconds [12]. The longer measurement time is, the more likely blood pressure is to increase due to an increase in peripheral vascular resistance caused by static movement and occlusion of circulation as a result of mechano reflex, metaboreflex and other actions [18-22]. The maximal muscle strength in our study reached its maximum after 2 seconds had passed for all participants but did not decrease until 20 seconds had passed. Therefore, it is possible to measure maximum muscle strength with the same measurement time (5 seconds) as handgrip strength, instead of 10 seconds.
Conclusion
By measuring pinch endurance, both the elderly and the younger groups showed no difference in transition of strength until 19 seconds and were able to exert a constant strength. The younger group showed a decline after 20 seconds onwards. The results may be useful as a reference for sustaining strength when exerting the maximum pinch strength in daily life and sports. We would like to continue to study the effect of sustained force on circulatory hemodynamics, the comparison of strength with key pinch and others, and the relationship with hand coordination.
Acknowledgement
None.
Conflict of Interest
None.
References
- Balla C, Passarini G, Bonsi B, Pavasini R, Tonet E, et al. (2021) Physical performance status predicts mortality in aging patients undergoing pacemaker implantation. J Cardiovasc Med 22(10): 738-743.
- Genest F, Lindstrom S, Scherer S, Schneider M, Seefried L (2021) Feasibility of simple exercise interventions for men with osteoporosis - A prospective randomized controlled pilot study. Bone Rep 24(15): 101099.
- Keller JL, Kennedy KG (2021) Men exhibit faster skeletal muscle tissue desaturation than women before and after a fatiguing handgrip. Eur J Appl Physiol 13: 1-11.
- Samuel TJ, Haykowsky MJF, Sarma S, Nelson MD (2019) Diastolic Stress Testing: Have You Considered Isometric Handgrip Echocardiography? JACC Cardiovasc Imaging 12(10): 2095-2097.
- Iwata K, Kitai T, Yoshimura Y, Honda A, Shimogai T, et al. (2021) Clinical impact of functional independent measure (FIM) on 180-day readmission and mortality in elderly patients hospitalized with acute decompensated heart failure. Heart Vessels 36(10): 1536-1541.
- Lai JC, Tandon P, Bernal W, Tapper EB, Ekong U, et al. (2021) Malnutrition, Frailty, and Sarcopenia in Patients with Cirrhosis: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 74(3):1611-1644.
- Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, et al. (2020) Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc 21(3): 300-307.
- Buch A, Marcus Y, Shefer G, Zimmet P, Stern N (2021) Approach to Obesity in the Older Population. J Clin Endocrinol Metab 106(9): 2788-2805.
- Dorhout BG, Doets EL, van Dongen EJI, de Groot LCPGM, Haveman-Nies A (2021) In-depth analyses of the effects of a diet and resistance exercise intervention in older adults: who benefits most from ProMuscle in Practice? J Gerontol A Biol Sci Med Sci 1-9.
- Dunn JA, Koch-Borner S, Johanson ME, Wangdell J (2021) Toward Consensus in Assessing Upper Limb Muscle Strength and Pinch and Grip Strength in People with Tetraplegia Having Upper Limb Reconstructions. Top Spinal Cord Inj Rehabil 27(3): 70-82.
- El-Gohary TM, Abd Elkader SM, Al-Shenqiti AM, Ibrahim MI (2019) Assessment of hand-grip and key-pinch strength at three arm positions among healthy college students: Dominant versus non-dominant hand. J Taibah Univ Med Sci 14(6): 566-571.
- Miyahara S, Tanikawa Y, Hirai H, Togashi S (2021) Handgrip Endurance in Healthy Elderly People. ABEB 5(3): 1-4
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE , et. al. (2017) 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 70(6): 776-803.
- Alahmari KA, Kakaraparthi VN, Reddy RS, Silvian PS, Ahmad I, et al. (2019) Percentage difference of hand dimensions and their correlation with hand grip and pinch strength among schoolchildren in Saudi Arabia. Niger J Clin Pract 22(10): 1356-1364.
- Kataoka H, Miyatake N, Kitayama N, Murao S, Kohi F, et al. (2016) Relationship of toe pinch force to other muscle strength parameters in men with type 2 diabetes. Environ Health Prev Med 21(4):179-185.
- Lam NW, Goh HT, Kamaruzzaman SB, Chin AV, Poi PJ, et al. (2016) Normative data for hand grip strength and key pinch strength, stratified by age and gender for a multiethnic Asian population. Singapore Med J 57(10): 578-584.
- Rostamzadeh S, Saremi M, Vosoughi S, Bradtmiller B, Janani L, et. al. (2021) Analysis of hand-forearm anthropometric components in assessing handgrip and pinch strengths of school-aged children and adolescents: a partial least squares (PLS) approach. BMC Pediatr 21(1): 39.
- Schmidt H, Francis DP, Rauchhaus M, Werdan K, Piepoli MF (2005) Chemo- and ergoreflexes in health, disease and ageing. Int J Cardiol 98(3): 369-378.
- Scott AC, Francis DP, Davies LC, Ponikowski P, Coats AJ, et al. (2000) Contribution of skeletal muscle 'ergoreceptors' in the human leg to respiratory control in chronic heart failure. J Physiol 529 Pt 3(Pt 3): 863-870.
- Vorluni L, Volianitis S (2008) Baroreflex control of sinus node during dynamic exercise in humans: effect of muscle mechanoreflex. Acta Physiol (Oxf) 192(3): 351-357.
- Hureau TJ, Weavil JC, Thurston TS, Broxterman RM, Nelson AD, et al. (2018) Identifying the role of group III/IV muscle afferents in the carotid baroreflex control of mean arterial pressure and heart rate during exercise. J Physiol 596(8): 1373-1384.
- Lis A, Lopusiewicz W, Piepoli MF, Ponikowska B, Paleczny B (2020) Passive bilateral leg cycling with concomitant regional circulatory occlusion for testing mechanoreflex-metaboreflex interactions in humans. Clin Auton Res 30(6): 549-556.
-
So Miyahara, Yoshihiro Tanikawa, Hideo Hirai, Akira Otsuka, Seiji Togashi. Pinch Endurance in Elderly People. Arch Biomed Eng & Biotechnol. 6(1): 2021. ABEB.MS.ID.000627.
-
Pinch Endurance, Elderly, Clinical criteria, Handgrip endurance, Malignant, Healthy young people
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






