 Research Article
Research Article
Comparison of the Effectiveness of the Minimally Invasive Approach with Preserved Piriformis Muscle with the Standard Posterolateral Approach in Total Hip Arthroplasty
Tiemure Wu1, Luis Oscar Marrero Riveron1, Ricardo Jesus Tarragona Reinoso1, Horacio Tabares Neyra2*
1International Orthopedic Scientific Complex, Frank País, Cuba
2Center for Research in Longevity, Aging and Health, Cuba
Horacio Tabares Neyra, Center for Research in Longevity, Aging and Health, Cuba.
Received Date: March 14, 2023; Published Date: April 19, 2023
Summary
Objective: The purpose of this study is to determine if the minimally invasive posterolateral approach with preserved piriformis muscle is superior to the conventional technique in total hip arthroplasty.
Methods: A prospective, randomized study was carried out where the sample was made up of 200 patients who underwent primary total hip arthroplasty between September 2019 and March 2021 with a minimum follow-up of one year at the Beijing Jishuitan Hospital. Perioperative bleeding, postoperative pain, recovery time, component orientation, size, and fit, frequency of complications, and functional outcome were evaluated.
Results: No significant differences were found between the groups in terms of perioperative bleeding, operation time. Recovery speed was significantly higher with the minimally invasive posterolateral approach, as earlier onset of ambulation and shorter hospital stays were detected. In the minimally invasive surgery group, the acetabular components were more anteverse, the size of the acetabular component and femoral head was smaller, the adjustment technique was predominantly press fit, and the Visual Analogue Scale score was significantly lower at 48 hours. postoperative No differences were found in terms of the frequency of complications or functional results at one year.
Conclusions: The minimally invasive approach with preserved piriformis muscle achieves faster recovery and early pain relief compared to the conventional approach, with a functional result similar to that of conventional techniques in 12 weeks
Abstract
Objective: The purpose of this study is to determine if Mis-PLA is superior to the conventional technique in total hip arthroplasty.
Methods: A prospective, randomized study was carried out where the sample constitutes 200 patients who underwent primary THA between september 2019 and march 2021 with a minimum follow-up of one year. Perioperative bleeding, postoperative pain, recovery time, component orientation, size, and fit, complication rate, and functional outcome were evaluated.
Results: No significant differences were found between the groups in terms of perioperative bleeding, operation time. The speed of recovery was significantly higher with the minimally invasive posterolateral approach, as an earlier onset of ambulation and a shorter hospitalization time were detected. In the Mis-PLA group, the acetabular components were more anteversion (p = 0.003), the size of the acetabular component and femoral head was smaller, the fitting technique was predominantly press-fit, the Visual Analogue Scale was significantly lower at 48 hours postoperatively. No differences were found in terms of complication rate or functional outcome at one year.
Conclusions: The Mis-PLA achieves faster recovery and early pain relief compared to the conventional approach without compromising surgical time, component orientation, or increasing the rate of complications, with functional results similar to conventional techniques in 12 weeks.
Keywords: Total hip arthroplasty; Posterolateral approach; Minimally invasive surgery; Mis-PLA
Introduction
Since it entered the field of orthopedics, total hip arthroplasty has become one of the most successful surgeries due to its good effect on diseases around the hip joint [1-3]. In an early period of time, the focus of surgery was primarily on the design, material, and fixation of the prosthesis, but in recent decades more and more attention has been paid to the surgical approach [4].
The traditional posterolateral approach has a stable and good effect in hip arthroplasty, in the United States, the posterolateral (Moore/Southern) approach is the most common surgical approach for primary and revision total hip arthroplasty [5]. This approach provides excellent exposure of the proximal femur and acetabular anatomy, but also carries an increased risk of neurovascular injury and dislocation of the prosthesis [4,6].
Minimally invasive surgeries will become more frequent because their safety has been repeatedly demonstrated with different approaches [7,8]. The pressure for smaller-incision surgery is coming from patients, and current studies suggest that patient satisfaction with minimally invasive surgery is high [9]. A small incision gives them more hope that the result they envision will be achieved. Patients want pain relief and they want to achieve their functional goals, but true satisfaction is not achieved without achieving their psychosocial goals, the most important of which is that they do not want to be self-conscious about their hip [10]. They want to regain control of their independence and activities, which their disability limits. Patients intuitively believe that the smaller incision will cause them less injury, allowing for a quicker recovery, they also correlate the smaller incision with less violation of their body, which means a better chance of full recovery. A more aesthetic wound is the objective reference for the subjective expectations of the patient [11].
The minimally invasive posterolateral approach with preserved piriformis muscle (Piriformis-sparing minimally-invasive approach, Mis-PLA) is a rarely reported approach, according to the author’s experience, until now very few articles can be found in Pubmed. In 2006, Khan et al. first reported Mis-PLA [12]. Compared to the traditional posterior approach, this approach shows a faster restoration of hip function. Biomechanical studies performed by Snijders et al. and Giphart et al [13,14]. demonstrated that the piriformis muscle is important for hip stability and function, and a randomized controlled trial of 89 cases by Khan et al. further confirmed the superiority of this procedure in the early postoperative period [15]. Studies have found that the function and stability of the hip joint are related to the piriformis muscle [16]. Therefore, the minimally invasive posterolateral approach with preserved piriformis muscle is an easy approach to proceed, beneficial for the recovery of joint function, and the frequency of dislocation is lower [15, 17-19].
Despite the novelty of the previous studies mentioned, this study investigated the effectiveness of the minimally invasive posterolateral approach with preserved piriformis muscle and the posterolateral approach, in order to determine whether Mis-PLA is superior to the standard technique in total arthroplasty. Hip. The objective of this study was to compare the results obtained using the Mis-PLA and standard posterolateral approaches in terms of perioperative bleeding, postoperative pain, speed of recovery, surgical time, orientation and adjustment of implanted components, frequency of complications, and functional outcome.
Materials and methods
General aspects of the study
A prospective, randomized study was carried out where the sample constituted 200 patients who underwent primary uncemented CTA between September 2019 and March 2021 at the Beijing Jishuitan Hospital, with a one-year follow-up from the arthroplasty and who met the following inclusion criteria: 1 - Age over 18 years. 2 - Diagnosis of primary or secondary coxarthrosis such as congenital hip dysplasia, avascular necrosis of the hip, ankylosing spondylitis. The following were excluded from the study: 1- Patients with revision total hip arthroplasty. 2 - Patients with a history of epilepsy, mental retardation, hemiplegia or movement imbalance. 3 - Patients with a history of hip infections. 4 - Suffering from diseases that could seriously affect postoperative functional recovery, such as severe knee arthropathy and severe spinal disease. 5 - Patients with benign or malignant neoplasm of the hip joint. The patients were randomly divided into two groups of 100 patients. The patients were randomly divided into two groups of 100 patients.
Clinical data
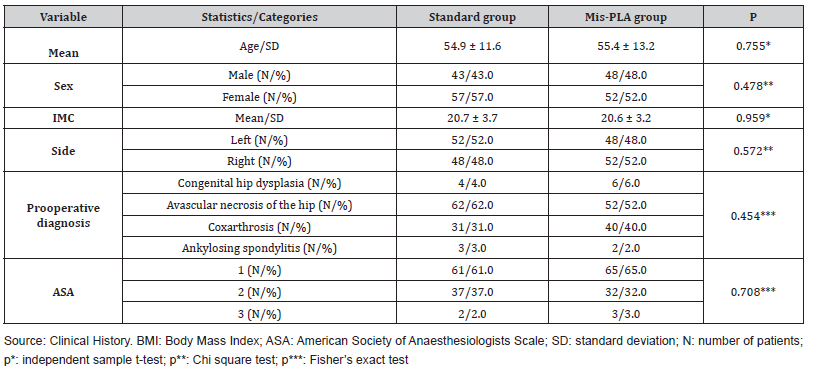
The patients were randomly divided into a posterolateral approach group (standard group) and a minimally invasive posterolateral approach group with preserved piriformis muscle (Mis-PLA Group), there were 100 cases with 100 hips in the standard group, including 43 men and 57 women, and the age was (54.9±11.6) years, among them, there were 31 cases with coxarthrosis, four cases with hip dysplasia, 62 cases with avascular necrosis of the femoral head, and three cases with ankylosing spondylitis. Mis-PLA group consisted of 100 cases with 100 hips, 48 men and 52 women, age (55.4±13.2) years, 41 cases with coxarthrosis and 6 cases with hip dysplasia, 49 cases with avascular necrosis of the femoral head two cases with ankylosing spondylitis (Table 1).
Table 1: Exposure and comparison of the preoperative variables of both groups.
Surgical methods
All surgeries were randomly performed by the same three physicians. The prostheses used were from DePuy Synthes (The Orthopedics Company of Johnson & Johnson, Warsaw, Indiana, United States). Preoperative preparation: complete blood count, urinalysis, blood chemistry, coagulogram, tests for sexually transmitted diseases, C-reactive protein, erythrocyte sedimentation rate, electrocardiogram, chest and pelvic bone X-ray, scanogram, cardiogram, lower limb angiogram, and function test lung if necessary (over 60 years). The patient’s blood pressure was controlled at (120-135) / (80-90) mm Hg and blood glucose was controlled below 7.9 mmol/L prior to surgery. The skin was prepared, a urethral catheter was placed. The size of the prosthesis was measured according to anteroposterior radiographs of the affected hip. Spinal anesthesia was used, with intravenous infusion of second-generation cephalosporin antimicrobial drug (cefuroxime, 1.5g) 30 minutes before surgery, intravenous infusion of 1g tranexamic acid 15 minutes before surgery, local infiltration by plane before surgery. skin incision of a mixture (mixed solution) containing ropivacaine, epinephrine (1;10,000) and saline to reduce intraoperative bleeding and postoperative pain.
Posterolateral approach
Patient in lateral decubitus on the unaffected side, followed by disinfection methods and draping. A 10-14 cm incision was made from the medial portion between the iliac crest and the tip of the greater trochanter in line with the femoral shaft to the distal end of the shaft.
The skin, subcutaneous tissue, and underlying fascia of the tensor fasciae latae were then incised plane by plane and a blunt dissection of the gluteus maximus was performed. The hip was then internally rotated to expose the piriformis muscle, the obturator internus muscle, the superior and inferior gastrocnemius muscles, and the quadratus thigh muscle. The muscle attachments were excised with an electric scalpel and the muscles folded upward to expose the joint capsule. Then, an inverted “T” shaped incision was made to open the joint capsule, the hip was dislocated, and the femoral neck was resected 1 cm above the lesser trochanter. The femoral head was then recovered using a special appliance with the femoral neck trimmed.
After cleaning the acetabular margin, the femoral head ligament was excised and residual soft tissues in the femoral head area were cleaned to expose the bony acetabulum. Trial acetabular prostheses of different sizes were placed to determine the ideal fit and bone coverage. An appropriate prosthesis was selected and placed in the acetabular cup in the position of 45° abduction and 15° anteversion, using screws for fixation if necessary. The affected limb was supported and adducted as much as possible. The proximal end of the femur was slotted and reamed to obtain the ideal size and the trial cast was placed. Lower leg length, range of motion, and hip stability were examined. The final prosthesis was placed for its reduction. A “mixed solution” was injected locally and the soft tissues sutured.
My-PLA
In the Mis-PLA group, after spinal anesthesia, the patient was placed in lateral decubitus on the unaffected side and a disinfection method was performed. A 7-9cm incision was made from the medial portion between the iliac crest and the tip of the greater trochanter in line with the femoral shaft to the distal end of the shaft.
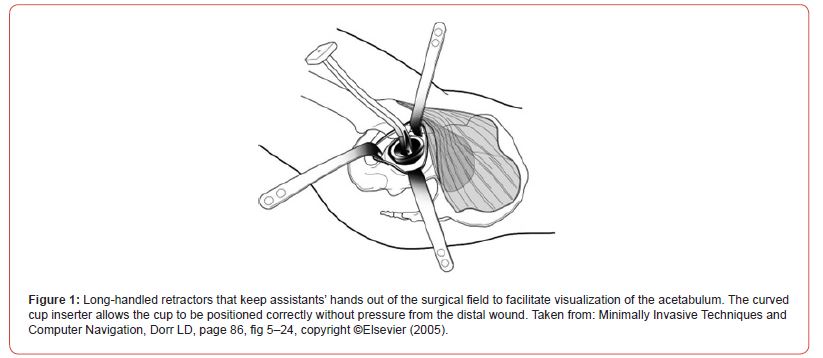
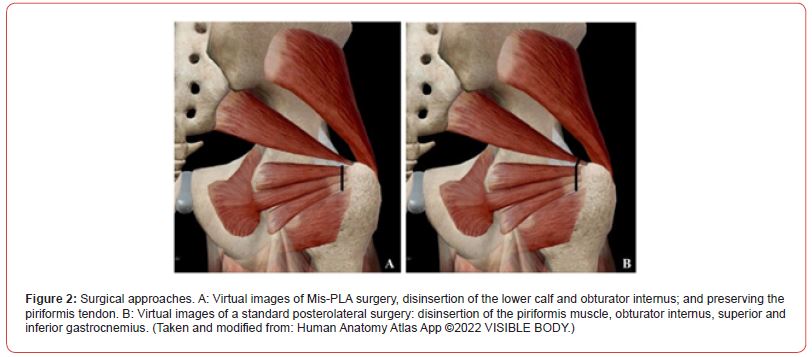
Next, the subcutaneous tissue and the underlying fascia of the tensor fasciae lata were incised, the sciatic nerve and gluteus medius were protected, and the special retractor was used to retract the piriformis muscle upwards (Figure 1), they were resected. the quadratus muscle, the superior gastrocnemius muscle, the obturator internus muscle, and the inferior gastrocnemius muscle. A vertical “L” shaped incision was made in the joint capsule. The tendon of the piriformis muscle and the posterior superior joint capsule were preserved. (Figure 2) A hip dislocation was then performed using internal rotation, hip flexion, and knee flexion. Femoral neck osteotomy was performed, and the femoral head was recovered with a special apparatus. The soft tissues of the acetabular socket and round ligament were resected, and the acetabular margin was cleaned to expose the bony acetabulum. Trial acetabular prostheses were implanted to determine ideal compatibility. An appropriate prosthesis was selected and placed in the acetabular cup and screws were used for fixation, if necessary (Figure 1,2).
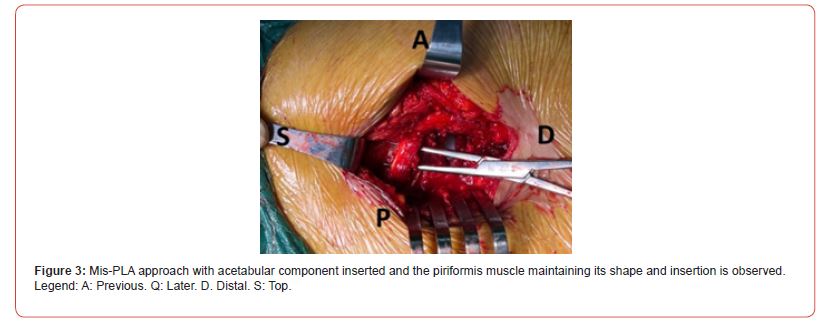
The affected limb was held and adducted as much as possible, the proximal end of the femur was reamed to obtain the ideal size. Then, the test cast was placed. Both lower limb length, range of motion, and hip stability were examined. The mixed solution was injected locally, the soft tissue around the bottom of the acetabulum was sutured. It was closed by plans (Figure 3).
Postoperative treatment, for both groups: General treatment: Both groups received analgesic pump for pain relief within 24 hours after the operation, and then switched to oxycodone and acetaminophen tablets(5mg+325mg)orally every day for one week after 24 hours with a dose of one tablet every 6 or 8 hours. Antibiotics were administered intravenously within 24 hours after surgery. Mis-PLA group: the affected limb was kept in a neutral position with slight abduction, and a pad was placed between the two legs to prevent adduction and internal rotation of the hip. Patients were instructed to perform isometric quadriceps exercises and ankle flexion and extension activities in bed the day after the operation to prevent deep vein thrombosis.
Data collection and monitoring
A Primary Data Collection Model (MPRD) was designed where the data provided in the interview and all the examinations performed on the patient in the pre, trans and postoperative period were collected. Harris Hip Score (HHS) and pain severity were assessed at preoperative visits. In the transoperative period, the measurement of surgical time, perioperative bleeding, and the size of the acetabular components and the femoral head were taken into account. In the postoperative period, pain was evaluated using the Visual Analogue Scale (VAS) at 48 hours and 12 months, speed of recovery, orientation of the acetabular component, frequency of complications, and the postoperative Harris Hip Score. the 12 months.
Statistical analysis
The SPSS 25.0 program (IBM, Armonk, NY, USA) was used for statistical analysis. The Kolmogorov-Smirnov test verified the normality of continuous variables. Normally distributed continuous data from the two groups were analysed using the t-test. For continuous data that were not normally distributed, the Mann-Whitney U Test was performed. To determine the association of qualitative variables, the Chi square test (χ2) was used. Fisher’s exact test was used to determine the association of qualitative variables in the case of expected frequencies less than 5. Primary follow-up results such as VAS were analysed using repeated measures analysis of variance (ANOVA). P < 0.05 was considered significant.
Result
In the present study, 200 patients with hip arthropathy who underwent THA were analyzed using different approaches, the sample was divided into two groups according to the approach modality. The control group underwent a posterolateral approach and the Mis-PLA study group, each consisting of 100 hips from 100 patients.
The value of the average age was 54.9 ± 11.6 years and the patients with the left side that occupies 52.0% in those treated with the classic posterolateral approach predominated. In the group treated with Mis-PLA, the mean age value was 55.4 ± 13.2 years and the right side predominated, occupying 52.0%. There was no significant difference in the mean age between the two treatment groups. Regarding BMI, the mean value in the standard group was 20.7 ± 3.7, and in the Mis-PLA group: 20.6 ± 3.2. When comparing both groups, no significant difference was observed. In both groups there was a predominance of female patients. In the group of patients treated with the standard posterolateral approach, these represented 57.0%, and in those treated with Mis- PLA, 52.0%. When comparing both groups, no significant difference was observed.
Regarding the preoperative diagnosis for the standard group, avascular necrosis of the hip represents the main cause that occupies 62.0%, coxarthrosis (31.0%), congenital dysplasia of the hip (4.0%), spondylitis ankylosing (3.0%). This is similar in the Mis- PLA group, with a predominance of hip avascular necrosis (52.0%), coxarthrosis (40.0%), decisive congenital dysplasia (6.0%) and ankylosing spondylitis. (2.0%). According to the American Society of Anaesthesiologist Physical Status (ASA) Classification, the two groups present a similar distribution: group one at 61.0%, group two at 31.0% and group three at 2.0% in the standard group, group one at 65.0%, group two at 32.0% and group three at 3.0% in the Mis-PLA group. When comparing both groups, no significant difference was observed (Table 1).
The exposure and comparison of the intraoperative and postoperative variables of both groups is presented in Table 2. The size of the acetabular component for Mis-PLA (49.8 ± 3mm) was smaller than for the standard group (52.3 ± 3.7mm). ) (p < 0.001). The femoral head component size for Mis-PLA (33.3 ± 2.8mm) was also smaller than for the standard group (34.5 ± 2.8mm) (p = 0.005). Regarding the adjustment techniques of acetabular components, the standard group shows more cases with screw adjustment (75.0%), the opposite of the Mis-PLA group, pressure adjustment occupies the majority (66.0%), and the difference was significant (p < 0.001).
Regarding the prosthesis position, the anteversion angle showed a significant difference in both groups. It was noticed that the Mis-PLA group presents a significantly higher degree of anteversion than the standard group (P = 0.020, Mann-Whitney U test). . The median grade was 17.4 (range 25-75%, 12.7-23.1) in the standard group and 21.6 (range 25-75%, 14.9-23.4) in the Mis- PLA group (Table 2, Fig.4). But regarding the abduction angle, the difference was not significant (p = 0.515).
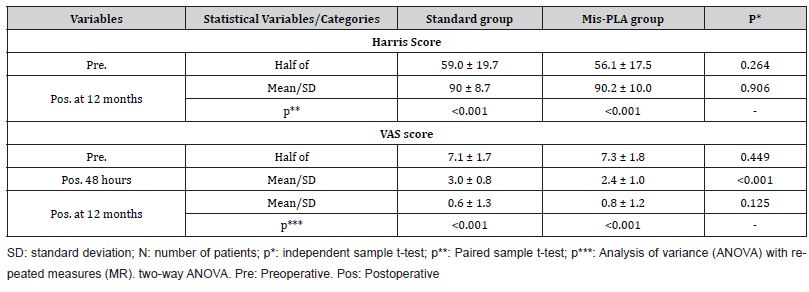
In the postoperative period, as can be seen in Table 3, the start of ambulation (day on which the patients were able to walk 10 continuous steps) was significantly better in the group of patients operated on using a minimally invasive approach (3.1 ± 2 .1) than the group with the classic posterolateral approach (3.9 ± 1.8) (p = 0.042). Hospitalization time (days) was significantly longer in the standard group (3.9 ± 0.9) than in the Mis-PLA group (3.3 ± 0.5) (p < 0.010). There was no significant difference between the Mis- PLA group and the standard group in terms of operating time (p = 0.221), intraoperative blood loss (p = 0.423), or number of screws (p = 0.652).
Regarding complications, the following complications occurred in the standard group: one case of dislocation after epileptic seizures and it was reduced under anesthesia, one case of hip bursitis that was alleviated when receiving conservative treatment. On the other hand, in the group of patients operated on using the Mis- PLA approach, a case was detected with hip dislocation after a fall, which was resolved conservatively without recurrence, one case suffered from sciatic pain that was controlled with analgesics and other conservative treatments, one case also suffered hip bursitis is improving at last moment to investigation by conservative treatment. After analyzing these data, no significant difference was found (p = 0.659) (Table 2).
Table 2: Exposure and comparison of the intraoperative and postoperative variables of both groups.
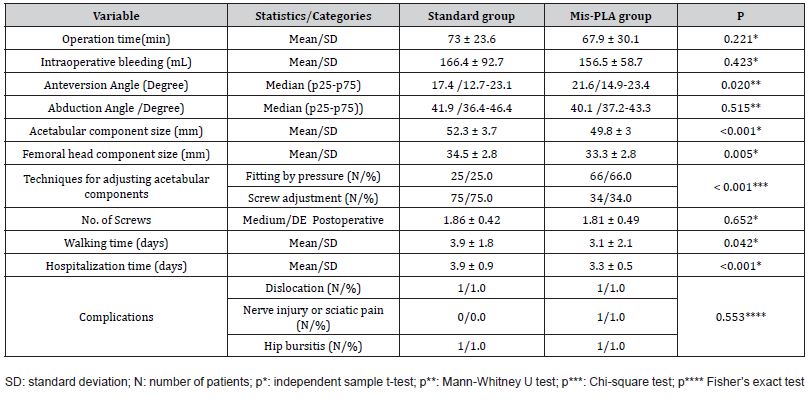
Table 3. In the evaluation of the functional result, the pre-surgical HHS was used and 12 months after the surgical intervention, a great improvement in joint function was observed, no difference was found between the two groups after 12 months. Regarding the VAS score, pain relief is observed in 48 hours and 12 months compared to the preoperative assessment. Regarding the intergroup comparison, it shows better pain relief in 48 postoperative hours in the Mis-PLA group (p < 0.001), which is not observed in 12 months (Table 3).
Table 3: Comparison of hip joint functions between two groups.
Discussion
Total hip arthroplasty is one of the most successful surgical procedures for relieving hip pain and improving quality of life and has been called “the operation of the 20th century.” Despite this success, early and late complications have been reported, and dislocation remains one of the most common early complications after THA. Historically, the posterior approach has been associated with a higher risk of dislocation compared to a lateral or anterior approach. Careful reconstruction of the capsule and short external rotators may decrease the risk of postoperative dislocation. Kwon et al performed a meta-analysis to determine the frequency of dislocations using a posterior approach with and without posterior soft tissue repair and found an eight-fold increased relative risk of dislocation when soft tissue repair was not performed [20].
The rotator muscles are important for the stability of the hip joint. Roche et al. 16 in their study of cadavers report that the piriformis muscle seems to act as a posterior stabilizer of the joint at 90° of flexion and, therefore, allow the an intact tendon can decrease the risk of dislocation and should not compromise access to the intramedullary canal through the posterior approach in CTA. In a two-year study conducted by Khan et al. [21]. in patients receiving THA through the standard posterolateral approach and Mis-PLA, who underwent magnetic resonance imaging three months and two years after surgery to determine the degree of deterioration of the piriformis muscle. The study determines that patients who undergo THA with the Mis-PLA approach have much less muscle deterioration, therefore, they conclude that the Mis-PLA approach damages the piriformis muscle less compared to the standard posterolateral approach. However, the cadaveric study carried out by Amanatullah et al. demonstrates, during the THA procedure using the Mis-PLA approach, the soft tissue damage that occurs outside the surgical field during the retraction of the unreleased muscles, such as the muscle piriformis is common, it is considered as an uncontrolled surgical variable [22]. The evaluation of Amanatullah 22 is in human cadavers, while the study of Khan et al [21]. is carried out ATC in living patients, therefore, there are obvious differences in muscle physiology with respect to the strength and laxity of the piriformis muscle during each test. procedure.
In this study, age, sex, BMI, side, operation time, bleeding did not present a significant difference. According to the study by Roche et al., the confusion between the trochanteric fossa and the piriformis fossa is what has led to the misunderstanding regarding the insertion of the piriformis tendon, and to the erroneous opinion that adequate access for CTA is not possible without resection. the piriformis tendon [16]. Actually, when comparing the Mis-PLA approach with the posterolateral approach, the surgical procedures are similar, so it is considered an easy technique to familiarize with and the learning curve is shorter, special retractors with long handles can be used that They form a 90° angle with the blade. These instruments keep the assistants’ hands off the field and place less stress on the soft tissues. In an unusual situation, without the use of special instruments, the purpose can also be achieved by placing a sharp Hohmann retractor under the posterior border of the gluteus medius and proximal to the piriformis tendon, which can be easily identified under visualization or by palpation. Therefore, for an experienced surgeon, the cost of time and perioperative bleeding may not make much of a difference. A similar result is also reported by Varela et al. [17].
In the prosthesis position, the anteversion angle comparison presents a significant difference and is larger in the Mis-PLA group. The converse was not found in the abduction angle comparison. However, in both groups the mean positions of the components were within the safe zone of Lewinnek [23]. In the work of Khan et al. it is reported that the acetabular components were less anteverted and had a lower mean angle of inclination in the Mis- PLA group. On the contrary, the study by Wang et al. demonstrates in their study that no significant difference was found in the angle of abduction or anteversions [24]. The author considers that due to the different technical details of the surgical operation and the different surgical tools, there may be some differences in the results, most importantly that they are within the Lewinnek safe zone.
When comparing the size of the acetabular component and the femoral head component, it is observed that the size of the prosthesis was significantly reduced in the Mis-PLA group. The author wants to argue that the patients are randomly distributed, and by this division, by chance, the size of the components is smaller in the Mis-PLA group. Regarding the adjustment techniques of acetabular components, the Mis-PLA group prefers pressure adjustment over screws. The authors of this research consider that the reduced surgical field affects the surgeon’s decision to some extent.
In the present investigation, the authors did not find significant differences in the functional result 12 months after surgery, having assessed the Harris Hip Score and VAS, but the VAS score at 48 postoperative hours was significantly lower in the group My-PLA. Although there are authors who demonstrate a better functional result, such as Wang et al., they reported that at three postoperative weeks a significant improvement is observed in hip functional assessment, but at eight weeks they found no significant difference [24]. Varela et al. made a comparison in three months and 12 months and did not find a significant difference either [17]. The study conducted by Brady and colleagues with a 10-year followup concluded that the Mis-PLA approach offered the same longterm functional benefits as the standard posterolateral approach. Therefore, the authors of this study consider that this procedure does not provide significant functional improvement in the long term, [15,25,26] but it is beneficial in the short term. This shortterm effect is also observed in walking time, and hospitalization time, which were significantly better in the group of patients operated using a minimally invasive approach. The authors of this research believe that the less soft tissue damage, the faster the patient’s recovery after surgery. Similar results are also reported by Varela et al. and Wang et al [17,24].
As stated in the results chapter, no significant differences were found in the frequency of any of the complications found between the Mis-PLA and conventional approaches. None of the consulted studies detected a higher frequency of complications with Mis-PLA surgery [15,17,24,27].
Conclusion
The use of the minimally invasive posterior approach when performing primary total hip arthroplasty has been able to accelerate early recovery, decrease hospitalization time, and alleviate early postoperative pain compared to the standard posterolateral approach without compromising surgical time, surgical bleeding. , nor increase the frequency of complications, with a similar functional result in both approaches when evaluating the patients at 12 weeks.
Authors Contribution
p>• Conception and design: TW, LOMR, HTN p>• Analysis and interpretation: TW, LOMR p>• Literature search: TW, HTN p>• Article writing: TW, LOMR, RJTR, HTN p>• Statistical analysis: TW p>• Critical review of the article: TW, LOMR, RJTR, HTN p>• Final article approval*: TW, LOMR, RJTR, HTN p>• Overall Responsibility: TW p>* All authors read and approved the final version of the manuscript that was sent to the journal.Conflicts of Interest
The authors declare not to have any interest conflicts.
References
- Melton J (1993) Hip fracture; a worldwide problem today and tomorrow. Bone 14: S1-8.
- Silva DMW (2018) Diagnosis of osteoporosis; bone mineral density, risk factors, or both. EC Orthopaedics 9(7): 500-502.
- Choudhary D, Alam A (2018) Anti-osteoporotic activity of bioactive compounds from Iris germanica targeting NK-Kappa B. EC Pharmacology & Toxicology 6 (8): 665-678
- Lu DY, Shen Y (2020) Bone surgery, tissue and function repairs. EC Orthopaedics 11(3): 1-2
- Lu DY, Che JY, Putta S, Wu HY, Shen Y (2019) How to improve the quality of pharmacotherapy for bone diseases. EC Orthopeadicis 10 (6): 366-369
- Lu DY, Che JY, Shen Y (2018) Osteoporosis, importance for early diagnosis and treatment. EC Orthopaedics 9 (9): 624-625
- Lu DY, Che JY, Shen Y (2018) Clinical treatments of osteoporosis, how to target co-morbidities. EC Orthopaedics 9(11): 781-782
- Negm SH (2018) The possible protective role of powder cuttlefish bone, crab shell and eggshell on osteoporotic rats. J Food and Diary Science 9(10): 111-121
- Lu DY, Che JY, Yarla NS, Putta S, Shen Y (2019) Bone disease recovery strategies, An overview. EC Orthopaedics 10 (1): 1-3
- Moore N, Slater GL (2019) Surgical technique update: Slater modification of minimally invasive brostrom reconstruction. EC Orthopaedics 10 (5): 308-314
- Araujo JL (2018) The role of the orthopedic surgeon in preventing low back pain chronification. EC Orthopaedics 9(12): 809-812
- Harsini SM, Oryan A (2018) Bone grafting and the materials for using in orthopaedics. EC Orthopaedics 9(12): 822-833
- Lu DY, Lu TR, Putta S, Shen Y (2019) Bone disease treatments, math-therapeutic modality. EC Orthopaedics. 10 (3): 140-143
- Zweedijk R, Tylleman C, Schwind P (2020) Scoliosis and osteopathy. Acta Scientific Orthopaedics 3(9): 30-43
- Koleva IB, Yoshinov B (2020) Rehabilitation as an essential element in the clinical practice of orthopaedics and traumatology. Acta Scientific Orthopaedics 3(9): 44-46
- Ban J, Fock V, Aryee DN, Kovar H (2021) Mechanisms, diagnosis and treatment of bone metastases. Cells 10(11): 2944.
- Lu DY, Xu B (2021) Cancer bone metastasis, experimental study. Acta Scientific Orthopaedics 5(12): 1-3: 10.
- Leung PC (2014) Traditional Chinese medicine in orthopaedics-problems and future direction. Open J Therapy Rehibilitations 2 (1): 1-4.
- Che JY, Lu DY (2021) Acupuncture for bone disease treatment. EC Orthopaedics 12(1): 15-16
- Lu DY, Chen YZ, Lu DF, Che JY (2019) Patients care and nursery in different diseases. Hospice and Palliative Medicine International Journal 3(1): 28-30.
-
Tiemure Wu, Luis Oscar Marrero Riveron, Ricardo Jesus Tarragona Reinoso, Horacio Tabares Neyra*. Comparison of the Effectiveness of the Minimally Invasive Approach with Preserved Piriformis Muscle with the Standard Posterolateral Approach in Total Hip Arthroplasty. Arch Biomed Eng & Biotechnol. 7(2): 2023. ABEB.MS.ID.000659.
-
Total hip arthroplasty, Posterolateral approach, Minimally invasive surgery, Mis-PLA, Orthopedics, Proximal femur, Acetabular, Anatomy, Prosthesis
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






