 Case Report
Case Report
Chromosome 10 Q26.1 Deletion Syndrome in a Patient Diagnosed Postnatal and the Mother Support for the Prevention of Postnatal Depression
Beatris Cela Stan1, Monica Zlati2, Ariela Elena Banu1, Gabriela Gurau1, AL Trifan3, Violeta Sapira1, Mihaela Lungu1, Roxana Elena Bogdan Goroftei1, Oana Alexandru4, Simona Dana Mitincu-Caramfil1, Eva-Maria Elkan1*, Anamaria Ciubara1
1University of Medicine and Pharmacy, Dunarea de Jos Galați, Romania
2University Ștefan cel Mare Suceava, Romania
3Grigore T Popa University of Medicine and Pharmacy Iași, Romania
4University Emergency Hospital for Children Sfantul Ioan Galați, Romania
Eva-Maria Elkan, University of Medicine and Pharmacy, Dunarea de Jos Galați, Romania.
Received Date: January 04, 2022; Published Date: February 02, 2022
Abstract
In the last time due to the wide genetic methods of genetic mutation determination, a lot of rare syndromes were highlighted and described in detail so it could be made an anticipatory strategy for the child born with a known or even new genetic mutation. Many of those mutations are not inherited and not found in other family members so that it is important to elucidate for the child and family and for the future descendants the variety of evolution possibilities and to have in mind more medical scenarios after which the medical team can plan the interventions. Rehabilitation must start from first day of diagnosis and this must be integrated in a large vision of a multidisciplinary team and networks prepared for this. Planning helps doctors and families not to waste time and to give a stronger support to the mothers because they feel that their child can gain the abilities to have a good life and a good social integration. So, the courage of the mother is greater, and the mother will not confront with postpartum depression seeing the involvement and the competences of the medical team. Postpartum depression affects yearly more than 27,6% women worldwide. The way the team discussed and concluded about this rare entity the 10q26.1 mutation in a male patient decided the good outcome and the good care which the child has beneficiated.
Keywords: Chromosome 10q26.1; Children; Prevention; Postpartum depression; Genetic
Introduction
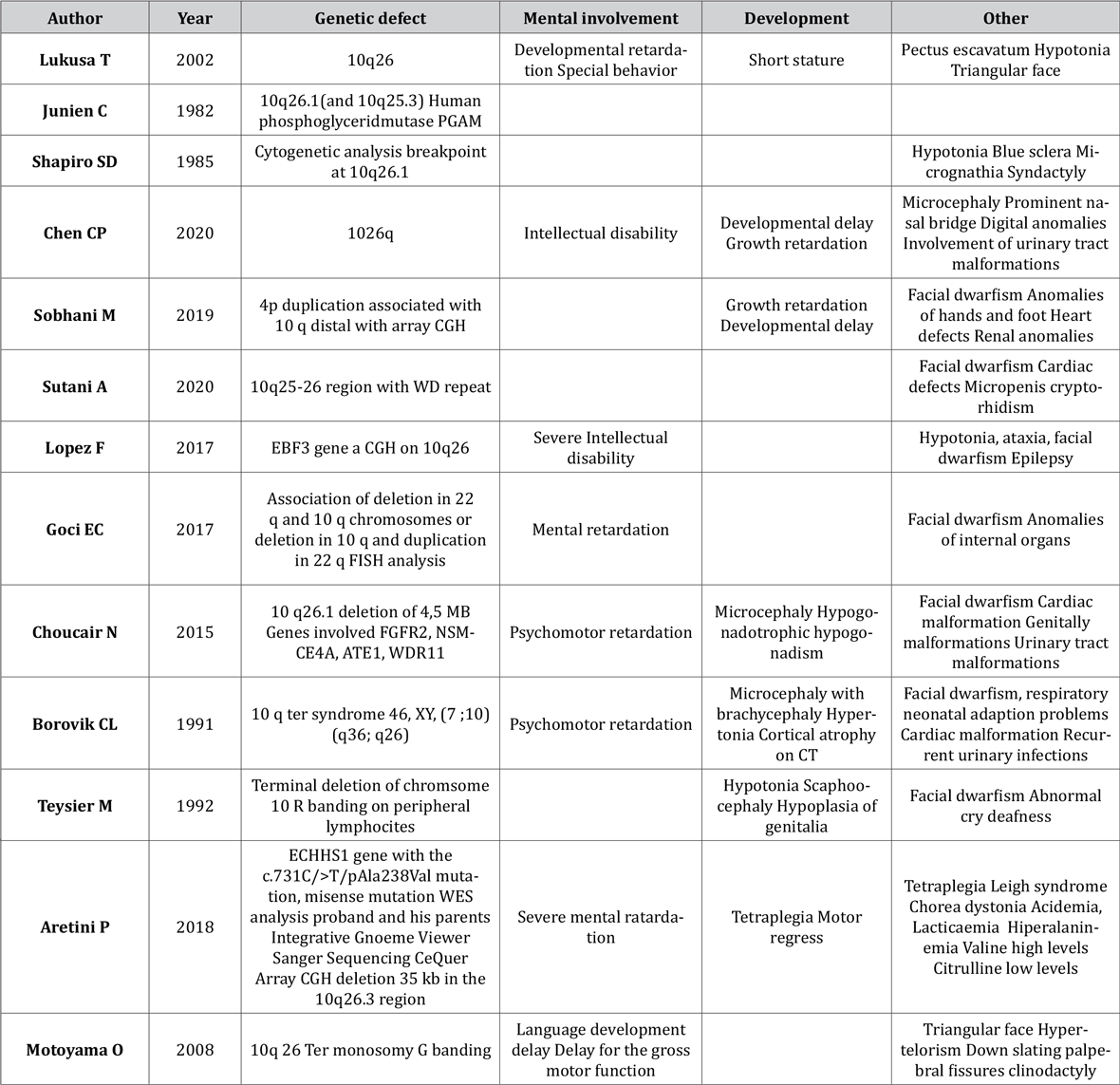
The karyotype of the patients with 10q deletion can be described making a comparison with the clinical aspect of the phenotype [1]. A syndrome due to the deletion at the level of the long arm of the chromosome 10 is defined in the more research [2]. Genetic polymorphism is a phenomenon which can be found because of tandem repeats of 14-65 base pairs thus can be seen also in the case of the chromosome band 10q26 [3]. Clinical detected facial dwarfism can be correlated with the dysfunction of the genes FGFR2, NSMCE4A, ATE1 but these genes can be also in tandem with heart defects [4]. At the level of the chromosome 10q26 region it is also located also the WD protein families which can have as a consequence the hypogonadotropic hypogonadism if we detect a defect in the WDR11 gene is detected [4,5]. In some cases, in the 10q Ter syndrome the mechanism is due to a paternal translocation and the resulting the genetic aspect being 46,XY, (7;10) (q36;q26) with the consequence of clinical facial dwarfism, cardio-respiratory involvement and hypertonia [6]. One method for the diagnosis of the genetic anomaly is the FISH analysis which shows the breakpoint and also helps to elucidate the extent of the deletion [7]. Another method is the array CGH, and an example is the elucidation of the trisomy 4p16.3p12 associated with 10q26.3 monosomy [8]. Also, with a CGH there was diagnosed 10q.26 deletions associated with EBF3 mutations which lead to small deletions of key amino acids [9]. For the detection of small chromosomal fragments (1-4 Mb) molecular techniques are welcome like FISH, MLPA or array CGH [10]. A new field is the genome editing with which there can be corrected various pathogenic mutations, but this raises a lot of bioethical aspects and so intervention in the human genome is closely tied up to eugenics [11]. Some studies are realized on the erythrocytes, so is the case for the Phosphoglycerylmutase which dysfunction can be linked to chromosome 10 26q.1. mutations involvement [12]. In some rare cases of congenital diaphragmatic defect with hernia the diagnosis is made prenatally elucidating in this way the association of 5q duplication with the terminal 10q deletion [13]. The situation of very rare cases brings an association between mutations of the 22q region and 10q making this in various combinations like distal monosomy 10q combined with distal trisomy 22, or other reverse models like distal monosomy of the 11q chromosome together with the distal trisomy 10 q [14].The breakpoint in 10q26 by found in the deletions of the chromosome 1o q can be made using peripheral lymphocytes and the technique of R banding and in one case of monosomy 10 q ter with the presence of deafness is a very rare event [15]. In this type of pathology with the involvement of the chromosome 10 26 q there are situations predisposing to bladder dysfunction and recurrent urinary infections due to vesicoureteral reflux and which cannot be related in extent to the neuropsychomotor involvement [16]. In Table 1 we present a meta-analysis of the genetic syndrome variants 10q26 (Table 1).
Table 1: Genetic variant in the 10q26 deletion syndrome.
Case Report
We want to present a case of 10q26.1 deletion syndrome detected postpartum in a child after seeing his facial dwarfism and making further genetic investigations which detected the chromosome 10q26.1 deletion. After genetic diagnosis the child underwent further investigation for the detection of other anomalies and exclusion of comorbidities.
The child was born from a pregnancy obtained by in vitro fertilization. A child of male gender was born at 36 weeks of gestation, birth weight 3190 and an APGAR score of 8. The birth was by caesarean section. A screening for Phenylketonuria, congenital hypthiroidism and audiology screening were performed at birth. Other prophylactic measures were performed like antihepatitis B vaccination and antituberculous vaccination after birth. The initial neonatal adaptation to extrauterine life was good. After birth were noted the dysmorphic status, bilaterally cryptorhidia and the presacrate fosetta. After the second day of life the child has had difficulties in feeding so the feeding was slowly effectuated and she have had a difficult coordination of the sucking and the swallowing reflexes, also with hypotonia and diminished spontan reaction as also associated with the spasticity of the members. From the beginning of the 5-th day of life the general status was better, the skin was of pink colour, and he developed subicter (he made phototherapy) and a systolic murmur of grade II/6 (precordial). The child din not needed therapy with oxygen. The child was put on alimentation with gavage and the digestive outcome was good at that moment. The child was also put on cardiovascular monitoring. The karyotype was taken at two weeks of age and the genetic exam was performed with the following conclusions: Newborn which was obtained with in vitro fertilization and under ultrasound surveillance. The pregnancy was tested with the Panorama test which concluded that the pregnancy was and without elements of genetic risk. The clinical aspect showed also craniofacial dwarfism and dolicocephalia, antimongoloid eyelids, nose with wide, prominent nose rood with visible columella. The ears are low inserted and malformated, detached ear flag. The child has also migrognatia, mamelon width, nipples with remote insert. The hands have abnormal dermatoglyphes. The child had also bilaterally cryptorhidia, and screed pit. Cardiac exam: Arterial canal persistence (shunt right left). The interatrial canal has 2 mm and maybe foramen ovale permeable. The tricuspid regurgitation of grade I. The systolic and diastolic function is normal. Transfontanelar echography: the cerebellar vermix is difficult to highlight the cerebellous hemispheres have a hypoechogenic aspect. Ophtalmologic exam: In observation hypoplasia of the optic nerve. In evolution he presents normal values of the hemoleucogram and a normal biochemical profile, with the exception of the inflammatory markers, and no clinical resonance and transitory raised values of the CK and LDH. In dynamic the evolution was slow favourable, and the digestive tolerance was with a progressive amelioration and after that the feeding was shifted from gavage to the syringe and afterthat to the nipple followed by a good coordination on the nipple feeding and ascendent wight curve. The primary cultures were sterile. Phenylkentoniuria negative. Screening for the congenital deafness: PASS audiometry on right ear, REFFER on the left ear. Transfontanelar echography in the 20-th day of life : hypoechogen cerebellum in totality. Neurologic exam: anterior fontanellae normotensive, Moro sign sketched, asymmetrically, moderate spasticity maintained on the limbs. At discharge Wight =060 grams, Length 50 cm, and discharged at 20 days of life. Lab tests: 2 days of life :fibrinogenemia=194,1 mg/dl, CRP=6 mg/Table 2 shows the evolution of the laboratory tests in dynamics (Table 2).
Table 2: Evolution of the laboratory tests in dynamics.
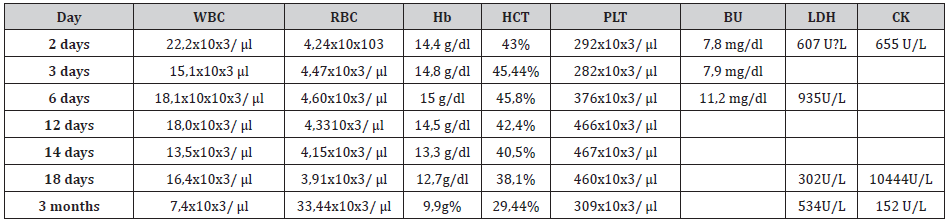
At 3 days of life other parameters were ALT(TGP)=16 U/L ST(TGO)=62U/L, NBIL=neonatal bilirubinemia=7,9 mg/dl, Cl=117 mmol/L Crea=1,0 mg/dL, K=4, mmol/L, Na=150 mmol/L, urea=19,6 mg/dL. In 4th day of life was made the gastric aspiration where no gram negative bacils, no gram positiv cocci an no Candida were detected. Also, the pharyngeal exudate was normal. But E.Coli was detected on the skin at the 4th day of life. At the same time hemocultures were sterile and the flora from the external auditory conduct was normal. . In the 6th day the hepatic parameters have had variations as also a hypoglicemic status, but the other parameters were good. ALT (TGP)=28 U/L AST (TGO) =112 U/L Ca=9,4mg/dl CK=130 U/L, CL=112mmol/l, Creatinine=0,5 mg/dl, glucose=29 mg/dl, MG=2,3 mg/dl, K+=6,1 mmol/l, Na=143 mmol/l, TRIG=122 mg/dl urea=16,0mg/dl Direct Bil=0,3 mg/dl, Neonatal bilirubinemiaaa =11,5 mg/dl. In the 8th day of life Escherichia Coli on the skin was detected in the 12-th day of life the procalcitonin was determined and the values were PCT=2,06 ng/ml in normal range. As also the other biologic parameter was normalized like transaminase, and the other were also normal. ALT(TGP)=19 U/L, AST(TGO)=40 U/L Cl=101 mmol/L, K=0,4 mmol/l, Na=140 mmol/l, fibrinogen 780,3 mg/dl. The gastric aspiration was repeated in the 13th day of life also normal and no bacils or candida detected. In the 14-th day of life Protein C was detected as 23 mg/L and fibrinogen at the level of 547,6 mg/dl. In the 18th day of life Protein C reactivity fell down to 10 mg/dl corresponding to the clinical status. Transaminase and CK have had a raising again. To values like % ALT(TGP)=144 U/L AST(TGO)=33U/L Ca=10,5mg/ dl, CK=10444 mmol/L LDH=302U/L with the other parameters in normal limit. Cardiologic exam at 1 month from clinical point of view normal Sinus rhythm normal =165 beats/minute and the axis +100 T wave neg in the precordial V1,V2,V3 derivations. Cardiologic exam must be repeated at the age of 1 year. Computer tomography of 3 Tesla at 2 months revealed Basal cisterns are normal Areas of the myelination corresponds to the age. The orbit, the orbital content and the optic chiasm is normal. The pituitary gland is normal at MRI. The enlargement of the endolymphatic duct at the internal right ear to a diameter at 2,4 mm cochlea and seemingly whole with 21/2 rotations. The internal left ear has not differentiation between cochlea and vestibulum and the formation of a cystic cavity of 6 mm and deformed semicircular channels. The ear flags inserted low, asymmetric. Enlargement of the vestibular aqueduct at the left ear. Common cavity at the level of the right ear. Transfontanelar echography at three months: The ventricular system is symmetrically, lateral ventricles of normal sizes. The distance between frontal horns is 26 mm (Normal values 27-32 mm) The transverse diameter at third ventricle <3mm. Corpus callosum normal. Resistivity index 0,68 (N=0,65-0,75) A repeated ophtalmologic exam at 3 months revealed hyperopic compound astigmatism at both eyes and delayed visual development for both eyes. Ophtalmologic exam was performed to evaluate the position of fixation the quality of fixation ant the time of fixation. So, the child follows inconstantly with both eyes. Right eye: Schiascopia with Tropicamide at the right eye +3.0DSf.+1.25 Dcil, Axis 180 grades. The eyelids and the appendages of the eyes have a normal status. At Biomicroscopy: The conjunctiva has a normal aspect. The cornea has a normal aspect. The crystalline has a normal aspect The iris of the eye has a normal aspect. The examination of the pupil revealed that the photomotor reflex and consensual reflex were normal. The anterior chamber of the eye has a normal aspect. Fundoscopy of the eye normal. The papilla is flat, pink, with clear outline. Indirect ophthalmoscopy : vessels of normal aspect, the macula is normal, the vitreous body is normal. The left eye Schiascopia with Tropicamide +3.0DSf.+1.00 Dcil, Axis 170 grades. The eyelids and the appendages of the eyes have a normal status. At Biomicroscopy: The conjunctiva has a normal aspect. The cornea has a normal aspect. The crystalline has a normal aspect The iris of the eye has a normal aspect. The examination of the pupil revealed is medium distended after mydriatic instillations and that the photomotor reflex and consensual reflex were normal. The anterior chamber of the eye has a normal aspect. Fundoscopy of the eye normal. The papilla is flat, pink, with clear outline. Indirect ophthalmoscopy: vessels of normal aspect, the macula is normal, the vitreous body is normal. The Krimsky test on both eyes: Ortoforia the deviation with prisms at a distance O AOF fc at almost O degrees at AOF fc.
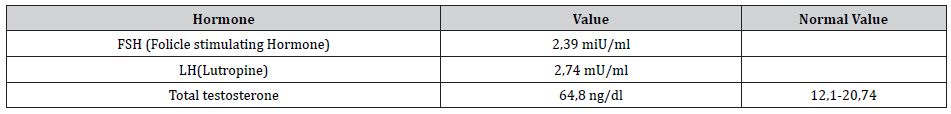
At three months an endocrinology evaluation was performed with the following values of the examined hormones as showed in (Table 3).
Table 3: The examinated hormones of the patient at three months.
The otorhinolaryngologic exam revealed at 3 ½: In observation Neurosensory hearing loss at the left ear. The maternity examination PASS right ear and REFFR left ear.so the test concluded DPOE-PASS on the right ear and REFER on the left ear. Tympanogram is type A on the Right Ear and type As on the Left Ear. Otomicroscopy T slightly mat bilaterally diffuse discrete congestion (through crying) on the left. MRI enlargement of the vestibular aqueduct on the left ear, malformation of the cochlea and of the vestibulum on the left, enlargement of the vestibular aqueduct on the right. Dysmorphic status with the external ear malformation bilaterally , malformation of the internal ear on the left side, Prematurity Neurosensorial hearing loss of the left ear Observation peripheric vestibular deficit possible walking gaining difficulties. In future it is needed to evaluate the auditory state responses ASSR vestibular evoked myogenic responses in later evaluations. Pediatric exam at 3 months: Weight =6105 grams, height=63 cm, 4 episodes of Urinary tract infections with Eschericia Coli, the first was febrile in December 2019 until 3 months of age. The child has physiologic fimosis grade 1.Tests bilaterally absent in the scrotum The torsion of the cavernous corps to the right BWT echografhc is 2 mm. Right kidneys absent from the renal lodge .Left kidney, without stones and with a clear cortico-sinusal delimitation. Echo structure was normal. Diameter in the long axis supination 6,2 cm/pronation 3,2 cm. Width of the renal cortex 11,3 cm. Central calyces dilated. Peripheric calyces nondilated. A-P diameter in renal pelvis in supination 9,7 intrarenal pelvis and 8,6 mm the extrarenal pelvis. A-P diameter in renal pelvis in pronation 9,7 mm with lombar urether 7,8 mm. Pelvian ureter can be seen 4,4/3,9 mm. Ultrasound of the bowel without stones in repletion. The width of the bladder walls is 2 mm Trranssonic content Regular outline. The indication is to make the micturition cystography and a DMSA (dimercaptosuccinic acid) scintigraphy. The therapy with Cefachlor 75m grams in the evening was started 125 mg/5 ml 2.5 ml in the evening, associated to treatment with Boniflor Immuno (Bifidobacterium animalis lactis and vitamin D) 10 drops /day in the food for 30 days and after that Enterolactis Baby (probiotic) 9 drops per day for other 30 days and after those Protects (Lactobacillus reuteri) 5 drops/day, in the next 30 days. The treatment with iron at the dose at 5mg/kg/day was started. It is necessary to make echography of the lombosacrate soft tissue to exclude the spina bifida oculta and to perform an abdominal MRI can see the tests if they can be seen in the abdomen. Surgical exam established at 3 months testicle not migrated in scrotum bilaterally. Abdominal MRI 3 Tesla exam revealed Liver with the antero-posterior diameter of the right lobe of 70 mm and the left lobe 36 mm, homogenous structure without focal lesions. The intrahepatic and extrahepatic billiary ducts of normally size nonexpanded. Gall bladder with greater volume with liquid content, plied on the fundus without stones in the lumen. The spleen with a bipolar axis of 61 mm present two cysts the greater one of 5 mm. The suprarenal glands and the pancreas are difficult to be identified because of the respiratory artefacts. Left hydronefrosis of grade I. The right kidney cannot be seen. There are not lymphadenopathy or free intraperitoneal liquid. IRM abdominal at 3 months and protocols of examination), 4 Tesla T1 COR, STR COR, AX T2AX. The right kidney cannot be seen as also the absence of the right renal artery is seen. The left kidney is present in the renal loge with the dimension of 29/27/63 mm (AP/TT/CC) and the thickness of the renal paarenchyma is 9.7 mm in normal position. The dilatation of the renal calyx is seen with the cranio-caudal diameter of the renal pelvis of 5.4 mm. Neurologic exam: at 3 months ½ revealed weight at 3 months and1/2 was 5400 grams. The anterior fontanelle was 2/2 cm normotensive, cranian perimeter of 37 cm, periroral cyanosis, left torticolis. Facial dwarfism revealed dolicocephalic aspect, antemongoloid orientation of the eyelids with slightly flattened root of the nose, down inserted ears. The lab exams revealed normal value of many parameters uric acid =1,6 mg/dl, ionic Calcium 4.95 mg/dl, Calcium 10.6 mg/dl, Creatinine 0.29 mg/dl, Glucose level in the blood 82,3 mg/dl, total proteins 6.0 g/ dl, transaminase slight modification of the values but with better evolution TGO(AST) 153 U/L, TGP (ALT) 56U/L, urea 15.2 mg/dl. The morphologic exam of the smear looks slight anisocytosis with rare polycromatophile elements. Uroculture is with Escherichia coli Infection. The child continued with Cefuroxime together with Simeticone 15 drops per day, Enterolactis (Lactobacillus paracasei) 9 drops/day. Echography of the hip: The right hip: the nucleus of the femural head. The cotiloid cavity the α angle of 69 grades, the βangle is of 50-degree, type 1-2 The left hip The nucleus of the femoral head it is not seen the cotiloid cavity with the α angle of 68 grades, the angle ẞ of 51 grade Type I normal Abdominal Echography The liver the right lobe is 74 mm (Nmax) 68 mm. Left lobe normal. The splenoportal axis was normal. The spleen has 46 mm (Nmax 50mm) the right kidney cannot be seen in the renal lodge. The left kidney has 57 mm the renal pelvis has calyx stems of 2 mm Endocrinologic exam: Testicles not palpable in the scrotum. Posterior dermal sinus. So the final diagnosis was 10q26.1 syndrome with 6,xy,del [10] q26.1, facial dwarfism, craniostenosis the persistent arterial canal, billaterally cryptorhidia, prolonged early jaundice, Feeding difficulties, Prematurity –Low age of gestation, unique kidneys, mild malnutrition, Infection with Escherichia coli of the urinary tract, feriprive anaemia, hepatocytolisis, anisocoria, nonmmigrated tests, hypermetropic compound astigmatism, both eyes development delayed visual development on both eyes posterior dermal synus. The child was rapidly evaluated form the birth and all the investigations were in a coordinated manner, so the parents understood the diagnosis and the care that the child needed, and the outcome was in a good manner and the dyad mother child functioned in the normal range.
Discussion
Sometimes the diagnosis is put just at the age of adolescent for the 10 del 26.1 with renal failure due to micromalformative aspects of the urinary tract [17]. New insights in molecular biology and cytogenetic shows that in the case of malignant transformations of the cells in the case of medulloblastoma and glioblastoma in children and in this situation the chromosome 10 is involved in 8-14% of cases more precisely the suppressor gene on the locus 10q23 being affected as also the gene MMAC1/PTEN localised on the din 10q26.3 segment [18]. Other genes are also located on the 10q chromosome in tumor genesis a role is played by the loss of the heterozygosity for the chromosome 10 thus leading to a higher grade of the astrocytoma, so the tumor suppression genes are PTEN, NEURL are located on this region [19] as also DMBT1 (10q25.3-26.1) which can suffer homozygous deletion, but this are events in low grade astrocytomas [20]. On the other hand, the possibility to diagnose rare diseases in adulthood can happen even if the first symptoms begin in early childhood and genetic diagnosis is put very late after onset. So, for example in the case of the mutation ECHHS1 gene together with a microdeletion of 35 kb in the 10q26.3 and the clinic picture of Leigh syndrome, without evident facial dwarfism in little childhood [21]. Another particularity is that it can happen that in this case it could be possible to find also Spina bifida as also testicle migrated in the abdomen so that abdominal MRI is better to be indicated in such cases. When the child has malformation from the birth the support of the mother is essential beginning from the first moment of the presenting the baby to the mum as also the adjustment of the mother child dyad. Many parents face the child diagnosis after birth even in Down syndrome sometimes and they can feel negative emotions and the mothers which have negative feelings are breastfeeding more difficult than mothers which do not experience. The breastfeeding stimulates the oral muscles of the child and brings benefit in mother-child communications and gives a better immune function tot the child thus feelings [22]. In the postpartum depression we must gain a good anamnesis to see if in the family of the mother there were other similar episodes at other births in relatives or the mother because after such episodes the mother may develop an episode of schizophrenia or bipolarity. Mental development of the child is influenced but the mother wellbeing so mental depression influences the development of the cognition in the child [23]. From the most ancient times the women have had a good perception about pregnancy and their life regimen as also their nutrition so culturally for the pregnant women it is always a good care in all cultures [24]. We can also see the rise and fall of CK in many newborns and in this case, we must have a very prudent attitude not to alarm the mother, different clinicians saying that repeated CK and LDH does not have sense, and we therefore insist to take them at different time interval weekly in the first month of life and after that monthly until 6 months so the clinician can interpret these values and indicate further investigations. CK can vary as value in the first days and weeks of life so further investigation of CK values is needed to rule out Duchenne Dystrophy and also some drugs can raise the CK levels in the neonate so their values can vary and that’s why repeated testing is needed [25]. A series of biologic parameters must be watched in children from families with a history of hypertension, cancer, dyslipidaemia or other diseases because in the case of children with dyslipidaemia decreased HDL cholesterol and increased LDL cholesterol can be associated also in the children with rare diseases or genetic disorders., because in every time a new combination of diseases not noted in the current literature is possible at every moment and we must keep that in mind [26] Delayed visual development must be suspected in all children with rare diseases so we must check more often for the development of visual anomalies in children with genetic syndromes because they can progress over time. Strabismus and amblyopia affect over 5-10% of the preschool children all over the worked. In children who are developmental delayed or have genetic syndromes there is necessary more frequent instrumental ophthalmologic screening because the risks to which these children are exposed to develop vision problems [27] Vestibular evoked myogenic responses and auditory state responses can be obtained by a wide range of frequencies 100-3200 Hertz, but a better response can be gained with the frequencies of 250-500 Hz. Amplitude modulated vestibular evoked myogenic responses: a study of carrier and modulating frequencies [28]. Many formulations in alimentation and in different plant products are used by families to have a better outcome in infections, burns, trauma so also the pregnant women can be exposed as also the child and the early pregnancy and later one, so parents are looking after products containing Cetraria islandica used in treating also viral infections especially those of the upper respiratory tract. But we must be very prudent in the indications of using plant formulation by pregnant women and after the birth when the family wants to give plant products to the baby to resolve the intercurrent problems like respiratory tract infections [29]. The wide range of use of antibiotics makes a switch in the intestinal flora of the mother thus also influencing the pregnancy outcome the most used antibiotics being Penicillins as also Cephalosporines and Fluoroquinolones. This is the reason why mother must be educated not to use self-medication in pregnancy [30]. Also, mother must be educated about the risks of the low weight born children to develop in time also tuberculous infection [31]. There are also situations when the mother can suffer from a cancer so she needs a psycho-oncologic support because anxiety and depression can vary in a very wide range for these patients and sometimes malignancies are discovered just in the pregnancy controls, so the mother has a double exposure to stress factors, the birth itself and a new diagnosis of a disease (cancer, diabetes, varicella, aso.) [32]. The blood group type is also important for the course of pregnancy in our case the group of the mother was with blood group type O and the child with blood type A and no antigenic reactions were observed, the O group is more often in the general population because it is the oldest blood group near 50% of the population having this type of blood group. But reactions mother child can involve the other 7500 antigens existing on the erythrocyte surface so the reactivity of the new-borns must be seen in the complexity of symptoms combinations and possibility of perinatal evolution [33]. A problem remains also the pregnancy in adolescents which can associate the polycystic ovarian syndrome underdiagnosed in the pregnancy period as also after birth the adaptation to the new role of motherhood so the combination of these can lead to difficulty to feed the child so the younger mothers must be sustained in gaining their new role [34]. Postanatal depression is in an incidence of 23,4%o of the women which were undertaken a post interview and detected in 27,6% of the women for prenatally depression [35]. In the case of the Panorama testing, it is revealed the fetal cfDNA from the mothers blood because it is a not invasive prenatal testing methods and so it can be detected the aneuploidy anomalies (like trisomy 21 or Turner syndrome) but some pathologies even with very careful testing cannot be detected so at each birth there remain a risk to discover diseases of the child not detected at the birth of the child [36]. Postnatal depression can be prevented using psychological and psychosocial intervention after the study of Dennis and Doswell (2015) and Morell (2016) that after birth the midwifery care must be extended to three months. But also, antenatal education is also a protective factor for the development of postnatal depression [37]. A known prevention protocol for postpartum depression is the Practical Resources for Effective Postpartum Parenting (PREPP). Postpartum in this intervention one target is to obtain a good sleep of the child and to reduce the fuss and crying behaviour of the child. Postpartum Depression can lead to marital discord and to impaired occupational and social functioning and these women can experience also panic attacks and anxiety in various degrees. The role of phone calls to those families is essential thus preventing o series of distorted perceptions about life situations and lowering the anxiety of the mothers [38].
Conclusion
In the postnatal period the precise investigation of the child gives the mother the certainty that her child has the best chances to develop. The medical team member must know each other before the child is born even if they are dispersed but they can reach each other via internet and mailing and other electronic facilities, so the diagnosis is complete, and each specialist is tied to the other ones. Time sparing and always reassurance of the mother that the child is under permanent surveillance and the access of the child’s family to all the specialists prevent anxiety, doubt and fear so the postpartum depression is prevented. Always a better outcome of a child means more security and more happiness in each family.
Acknowledgment
None.
Conflicts of Interest
No Conflict of Interest.
References
- Lukusa T, Smeets E, Vermeesch JR, Fryns JP (2002) Small terminal 10q26 deletion in a male patient with Noonan-like stigmata: diagnosis by cytogenetic and FISH analysis. Genet Couns 13(4): 417-425.
- Shapiro SD, Hansen KL, Pasztor LM, Di Liberti JH, R J Jorgenson, et al. (1985) Deletions of the long arm of chromosome 10. Am J Med Genet 20(1): 181-196.
- Colb M, Yang-Feng T, Francke U, Mermer B (1986) A variable tandem repeat locus mapped to chromosome band 10q26 is amplified and rearranged in leukocyte DNAs of two cancer patients. Nucleic Acids Res 14(20): 7929-7937.
- Choucair N, Abou Ghoch J, Fawaz A, Megarbane A, Eliane Chouery (2015) 10q26.1 Microdeletion: Redefining the critical regions for microcephaly and genital anomalies. Am J Med Genet A 167A(11): 2707-2713.
- Sutani A, Shima H, Hijikata A, Hosokawa S, Yuko Katoh-Fukui, et al. (2020) WDR11 is another causative gene for coloboma, cardiac anomaly and growth retardation in 10q26 deletion syndrome. Eur J Med Genet 63(1): 103626.
- C L Borovik, D Brunoni (1991) Terminal Deletion of Chromosome 10q26 due to a Paternal Translocation {(7;10)(q36;q26)} Am J Med Genet 41(4): 534-536.
- Lukusa T, Smeets E, Vermeesch JR, Fryns JP (2002) Small terminal 10q26 deletion in a male patient with Noonan-like stigmata: diagnosis by cytogenetic and FISH analysis. Genet Couns 13(4): 417-425.
- Sobhani M, Tahmasbi P, Nasiri F, Rahnama M, Roxana Karimi-Nejad, et al. (2019) A Patient with Trisomy 4p and Monosomy 10q. Arch Iran Med 22(7): 414-417.
- Lopes F, Soares G, Goncalves-Rocha M, Pinto-Basto J, et al. (2017) Whole Gene Deletion of EBF3 Supporting Haploinsufficiency of This Gene as a Mechanism of Neurodevelopmental Disease. Front Genet 8: 143.
- Butnariu L, Gramescu M, Caba L, Panzaru M, et al. (2017) Using of Multiple Chromosomal and Molecular Analyses to Elucidate the Etiology of Plurimalformative Syndromes. Rev Med Chir Soc Med Nat 121(3): 581-593
- Gorduza EV (2019) Genome Editing: Ali Baba's Treasure or Pandora's Box? Med Surg J - Rev Med Chir. Soc Med Nat 123(2): 213-216.
- Junien C, Despoisse S, Turleau C, De Grouchy J, Bucher T, Fundele R (1982) Assignment of phosphoglycerate mutase (PGAMA) to human chromosome 10. Regional mapping of GOT1 and PGAMA to subbands 10q26.1 (or q25.3). Ann Genet 25(1): 25-27.
- Chen CP, Huang JP, Chen SW, Chern SR et al. (2020) Prenatal diagnosis of concomitant distal 5q duplication and terminal 10q deletion in a fetus with intrauterine growth restriction, congenital diaphragmatic hernia and congenital heart defects. Taiwan J Obstet Gynecol 59(1): 135-139.
- Coci EG, Auhuber A, Langenbach A, Mrasek K, Joachim Riedel, et al. (2017) Novel Unbalanced Translocations Affecting the Long Arms of Chromosomes 10 and 22 Cause Complex Syndromes with Very Severe Neurodevelopmental Delay, Speech Impairment, Autistic Behavior, and Epilepsy Cytogenet Genome Res 151(4): 171-178.
- M Teyssier, C Charrin, J Dutruge, C Rousselle (1992) Monosomy 10qter: a new case. J Med Genet 29(5): 342-343.
- Motoyoma O, Tokuyama M, Uga N, Itaka K (2008) Urinary retention in a boy with terminal deletion of chromosome 10 q at band 26.1. Pediatr Int 50(4): 603-604.
- Leonard NJ, Harley FL, Lin CC (1999) Terminal deletion of chromosome 10 q, at band 26.1, follow-up in an adolescent male with high-output in an adolescent male with high-output renal failure from congenital obstructive uropathy. Am J Med Genet 86(2): 115-117.
- Mollenhauer J, Wiemann S, Scheurlen W, Korn B, Y Hayashi, et al. (1997) DMBT1 a new member of the SRCR superfamily, on chromosome 10q25.3-26.1 is deleted in malignant brain tumors. Nat Genet 17(1): 32-39.
- Terada K, Tamiya T, Daido S, Kambara H, Hiroaki Tanaka, et al. (2002) Prognostic value of loss of heterozygosity around thrre candidate tumor supressor genes on chromosome 10q in astrocytomas. J Neurooncol 58(2): 107-114.
- Fan X, Munoz J, Sanko SG, Castresana JS (2002) PTEN, DMBT1, and p16 alterations in diffusely infiltrating astrocytomas. Int J Oncol 21(3): 667-674.
- Aretini P, Mazzanti CM, La Ferla M, Franceschi S (2018) Next generation sequencing technologies for a successful diagnosis in a cold case of Leigh syndrome. BMC Neurol 18(1): 99.
- Da Silva RB, Barbieri-FigueiredoMC, Van Riper M (2019) (2018): Breastfeeding Experiences of Mothers of Children with Down Syndrome. Comprehensive Child and Adolescent Nursing 42(4): 250-264.
- Van den Bergh BRH, van den Heuvel MI, Lahti M, Braeken M, De Rooij SR, Entringer S, et al. (2020) Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci Biobehav Rev 117: 26-64.
- Nutrition de la femme enceinte, entre le concept et la pratique. Stuparu Crețu M; Nechita A, Bușila C. IRTUM - Institutional Repository of the Technical University of Moldova 2018.
- Sitzmann FC, Orth H (1983) [N-acetyl-cystein-(NAC)-activated creatinkinase (CK) and isoenzyme CK-MB in the serum of children] Monatsschr Kinderheilkd 131(8): 509-512.
- Bușila C, Stuparu-Crețu M, Barna O, Balan G (2017) Dysipidemia in children as a risk factor for cardiovscular disease. Biotechnology and Biotechnological Eqquipment 31(6): 1192-1197.
- Earley B, Fashner J (2019) Eye Conditions in Infants and Children: Vision Screening and Routine Eye Examinations. FP Essent 484: 11-17.
- Cabral de Oliveira A, Pereira LD, Colafemina JF, dDe Lemos Meneezes P (2014) Acta Oto-Laryngologic 134(8): 796-801.
- Patriche S, Ghinea IO, Adam G, Gurau G (2019) Characterization of Bioactive Compounds from Romanian Cetraria islandica (L) Ach Rev Chim.(Bucharest) 70(6): 2186-2191.
- Draganscu M, Iancu AV, Firescu D, Dumitiru Buzia O et al. (2016) Trends in Antimicrobials consumption and Antimicrobial Resistance in an Infectious Diseases Hospital from the South-Eastern Region of Romania. Farmacia 64 (5): 770-774.
- Banu EA, Nechita A, Elkan-Cojocaru EM, Baciu G, Alina Manole, et al. (2018) Risk of tuberculosis in low-birth-weight children from East Romania. Arch Med Sci 16(1): 162-166.
- Rebegea L, Firescu D, Baciu G, Ciubara AM (2019) Psycho-Oncology Support. BRAIN. Broad Research in Artificial Intelligence and Neuroscience 1(10): 77-88.
- Stuparu-Crețu M, Bușila C, Voinescu DC, Balan G (2018) The Correlations Between ABO Blood Type and the Metabolic Disorders in Adolescents with Polycystic Ovarian Syndrome. Rev Chim 69(9): 2467-2471.
- Stuparu-Crețu M, Bușila C, Caraman L, Balan G (2019) The Estimated Adolescents Carbohydrate Metabolism and Insulin Resistance in POCS. Journal of Chemistry 70(6): 2256-2260.
- Hobfoll SE, Ritter C, Lavin J, Hulsizer MR, Cameron RP (1995) Depression prevalence and incidence among inner-city pregnant and postpartum women. Journal of Consulting and Clinical Psychology 63(3): 445–453.
- Comas C, Echevarria M, Rodriguez MA, Prats P, Rodriguez I, et al. (2015) Initial experience with non-invasive prenatal testing of cell-free DNA for major chromosomal anomalies in a clinical setting. J Matern Fetal Neonatal Med 28(10): 1196-201.
- Mahdi A., Dembinsky M, Bristow K, Slade P (2019) Approaches to the prevention of postnatal depression and anxiety-a review of the literature. Journal of Psychosomatic Obstetrics & Gynecology 40(4): 250-263.
- Werner EA, Gustafsson HC, Lee S, Feng T, Jiang N, et al. (2016) PREPP: postpartum depression prevention through the mother–infant dyad. Arch Womens Ment Health 19(2): 229-242.
-
Beatris Cela Stan, Monica Zlati, Ariela Elena Banu, Gabriela Gurau, Eva-Maria Elkan. Chromosome 10 Q26.1 Deletion Syndrome in a Patient Diagnosed Postnatal and the Mother Support for the Prevention of Postnatal Depression. Arch Biomed Eng & Biotechnol. 6(3): 2022. ABEB.MS.ID.000638. DOI: 10.33552/ABEB.2022.06.000638.
-
Chromosome 10q26.1, Children, Prevention, Postpartum depression, Genetic, Anxiety, Depression, Turner syndrome, Aneuploidy, Aanomalies, Panorama testing, Cephalosporines, Fluoroquinolones
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






