 Review Article
Review Article
Bilateral Coronary Artery to Pulmonary Artery Fistulae: A Very Rare Anomaly
Jacob M Mathew1* and Kartik Shatagopam2
1Department of Cardiology, Salem Veterans Affairs Medical Center, USA
2Department of Cardiology, School of Medicine, Salem Veterans Affairs Medical Center, USA
Jacob M Mathew, Assistant Professor of Medicine, Virginia Tech Carilion School of Medicine, Department of Cardiology, Salem Veterans Affairs Medical Center USA.
Received Date:December 20, 2019; Published Date:January 28, 2020
Introduction
Coronary artery fistulas (CAFs) are a rare group of coronary anomalies which result in an abnormal connection between a coronary artery and either a cardiac chamber or any great vessel, most commonly pulmonary artery. They are mostly congenital but can be acquired and usually diagnosed incidentally. Although single vessel fistulas are far more common and have been reported routinely in literature, bilateral or multiple fistulas are extremely rare. Here, we describe a very unique case of bilateral coronary artery fistulas in a patient, with fortunately no significant hemodynamic consequences.
Case Report
Introduction
70 y/o male with a past medical history of diabetes, hypertension, hyperlipidemia, morbid obesity, family history of early coronary artery disease (CAD) and no known prior CAD who presented to the hospital for an episode of severe, sub-sternal chest pain associated with shortness of breath (SOB) and diaphoresis. Vital signs were normal, ECG and physical exam were unremarkable and lab work revealed normal CBC, serum chemistries, and negative troponins. Subsequently, patient underwent nuclear stress testing and was found to have a medium to large shadow, suggestive of possible ischemia or artifact in the lateral and basilar walls.
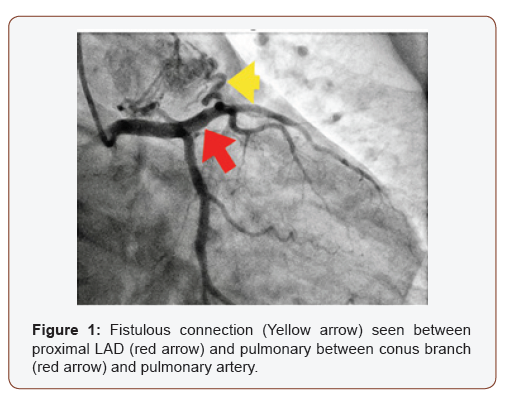
Left heart catheterization was then performed which revealed non-obstructive coronary arteries but other incidental coronary anomalies. On multiple views, there was noted to be a fistulous connection between the proximal left anterior descending artery (LAD) and the main pulmonary artery (Figure 1). A fistulous connection was also evident between the conus branch of the right coronary artery (RCA) to the main pulmonary artery (Figure 1 & 2).
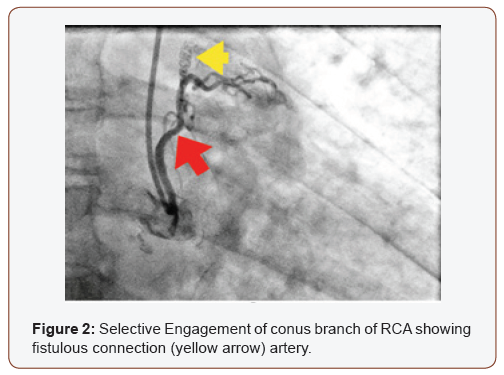
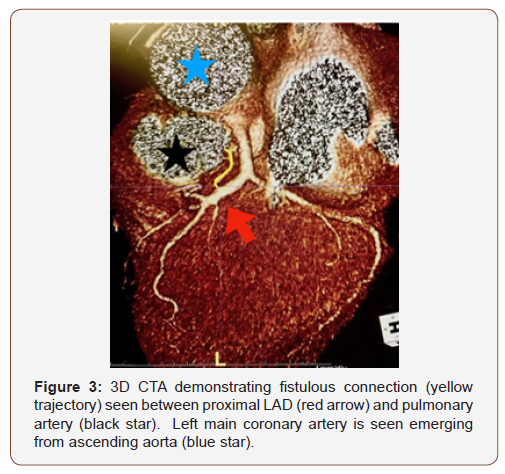
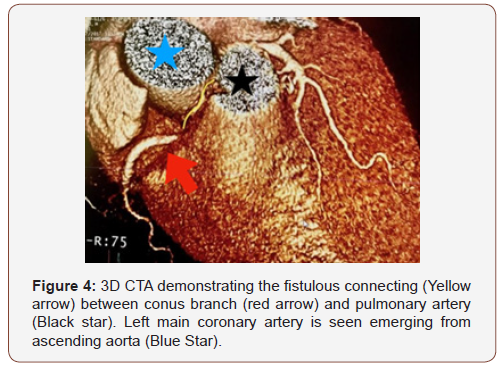
Right heart catheterization revealed mild pulmonary hypertension with the mean PA pressure of 27 mmHg. Cardiac index was normal at 2.38 L/min/m2. Oxygen saturation in right atrium (RA) was 62.7%, main pulmonary artery was 62.9%, right pulmonary artery was 62.4% and left pulmonary artery was 64.2%, suggestive of no significant mixing of blood secondary to left to right shunt. RA/right ventricular angiogram did not reveal any fistulous connection. Dedicated coronary CT angiogram was then obtained, which did show evidence of a small fistulous communication between the proximal LAD and the main pulmonary artery (Figure 3). A second fistula was seen between the conus branch and the main pulmonary artery (Figure 4).
Discussion
Coronary artery fistula (CAF), a major coronary anomaly by Ogden classification [1], is an abnormal connection between a coronary artery and any of the great vessels (pulmonary artery, superior vena cava, pulmonary veins or coronary sinus) or either of the cardiac chamber. First described by Krause in 1865 [2, 3], they are thought to arise due to the failure of intramyocardial trabecular sinusoids during the early embryonic period [4,5]. CAFs are most often congenital but can also be acquired from trauma, infection, iatrogenic injury (from congenital cardiovascular surgeries, catheter directed myocardial biopsy) [2,4].
A fistula arising from LAD and conus branch, with termination into the pulmonary artery, as in our patient, is an extremely rare finding [9]. CAFs are thought to be present in 0.002% of the general population, with single fistulas being most common and comprising 74% to 90% of all CAFs [4,6,7]. Multiple fistulas are significantly rarer, occurring in 10.7% to 16% of all CAFs, with involvement of both coronaries being less than 5% [4,6,7]. Drainage into pulmonary artery occurs with more frequency with bilateral fistulas (56%) than unilateral fistulas (17%) [8,9].
CAFs are typically found incidentally on coronary angiography, such being the case in our patient. With the advent of advanced CT angiography, prevalence of CAFs is increasing. In a retrospective study of 17,548 patients who underwent CTA of the heart, the incidence of CAF was 0.19% [10]. Pulmonary artery was found to be the most common site of drainage (84.8%) [10]. Most CAFs are small and do not result in significant hemodynamic issues or patient between proximal LAD (red arrow) and pulmonary RCA showing fistulous connection (yellow arrow) artery. between conus branch (red arrow) and pulmonary artery.
Complaints [12]. Large fistulas with significant flow can result in volume overload and pulmonary hypertension. Coronary ischemia can also result from excessive shunting of blood away from the coronary blood flow [12]. Most patients are asymptomatic, but significant fistulae can cause syncope or angina [12]. The main indications for closure for CAFs are patient symptoms, particularly congestive heart failure, coronary ischemia, or significant shunting [10]. Treatment options include observation, transcatheter embolization, or surgical intervention. Transcatheter closure, due to its less invasive nature is the primary modality recommended for symptomatic patients or asymptomatic patients with high risk findings for future complications, but surgical closure is preferred in complicated or tortuous cases [7,11]. In our patient, due to the asymptomatic nature of his bilateral fistulae, he was managed expectantly with regular outpatient cardiology follow up.
Conclusion
Coronary artery fistula (CAF) is a rare anomaly, most often congenital and usually found incidentally. Frequently, they are unilateral, and they arise from the left coronary system and empty into the pulmonary artery. We describe a very rare of bilateral coronary artery fistula to the pulmonary artery. Percutaneous closure or surgical closure are the preferred modalities of intervention in symptomatic patients.
Acknowledgement
None.
Conflicts of Interest
No Conflicts of interest.
References
- Dodge-Khatami A, Mavroudis C, Backer CL (2000) Congenital heart surgery nomenclature and database project: anomalies of the coronary arteries. Ann Thoracic Surgery 69(3 Suppl 1): 270-277.
- Rittenhouse EA, Doty DB, Ehrenhaft JL (1975) Congenital coronary artery -cardiac chamber fistula: review of operative management. Ann Thoracic Surgery 20: 468-85.
- Krause W (1865) About the origin of an accessory coronary artery from the pullmonalis artery. Z Ratl Med 24: 225-229.
- Huang YK, Lei MH, Lu MS, Tseng CN, Chang JP, et al. (2006) Bilateral coronary-to-pulmonary artery fistulas. Ann Thoracic Surgery 82: 1886-1888.
- (2012) Coronary artery Fistula. A Review. The Society of Thoracic Surgeons 93: 2084-2092.
- Fernandes ED, Kadivar H, Hallman GL, Reul GJ, Ott DA, et al. (1992) Congenital malformations of the coronary arteries: the Texas Heart Institute experience. Ann Thoracic Surgery 54(4): 732-740.
- Olearchyk AS, Runk DM, Alavi M, Grosss MA (1997) Congenital bilateral coronary-to-pulmonary artery fistulas. Ann Thoracic Surgery 64(1): 233-235.
- Liberthson RR, Sagar K, Berkoben JP, Weintraub RM, Levine FH (1979) Congenital coronary arteriovenous fistula. Report of 13 patients, review of the literature and delineation of management. Circulation 59(5): 849-854.
- Urrutia-S CO, Falaschi G, Ott DA, Cooley DA (1983) Surgical management of 56 patients with congenital coronary artery fistulas. Ann Thoracic Surgery 35: 300-307.
- K Zhou, L Kong, Y Wang (2015) Coronary Artery fistula in adults: evaluation with dual-source CT coronary angiography. Journal of Radiology 88: 20140754.
- Tirilmois T, Aleksic I, Busch T, Zemker D, Ruschewski W, et al. (2005) Congenital coronary artery fistulas in adults: surgical treatment and outcome. Int J Cardiology 98(1): 57-90.
- Challoumas D, Pericleous A, Dimitrakaki IA, Danelatos C, Dimitrakakis G (2014) Coronary arteriovenous fistulae: a review. Int J Angiol 23(1):1-10.
-
Jacob M Mathew, Kartik Shatagopam. Bilateral Coronary Artery to Pulmonary Artery Fistulae: A Very Rare Anomaly. Arch Biomed Eng & Biotechnol. 3(4): 2020. ABEB.MS.ID.000570.
-
Bilateral Coronary Artery, Pulmonary Artery Fistulae, Congenital, Chest pain, Shortness of breath, Basilar walls, Coronary artery, Trauma, Infection, Iatrogenic injury
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






